Why the First Trimester Is the Most Important Time for Medication Safety
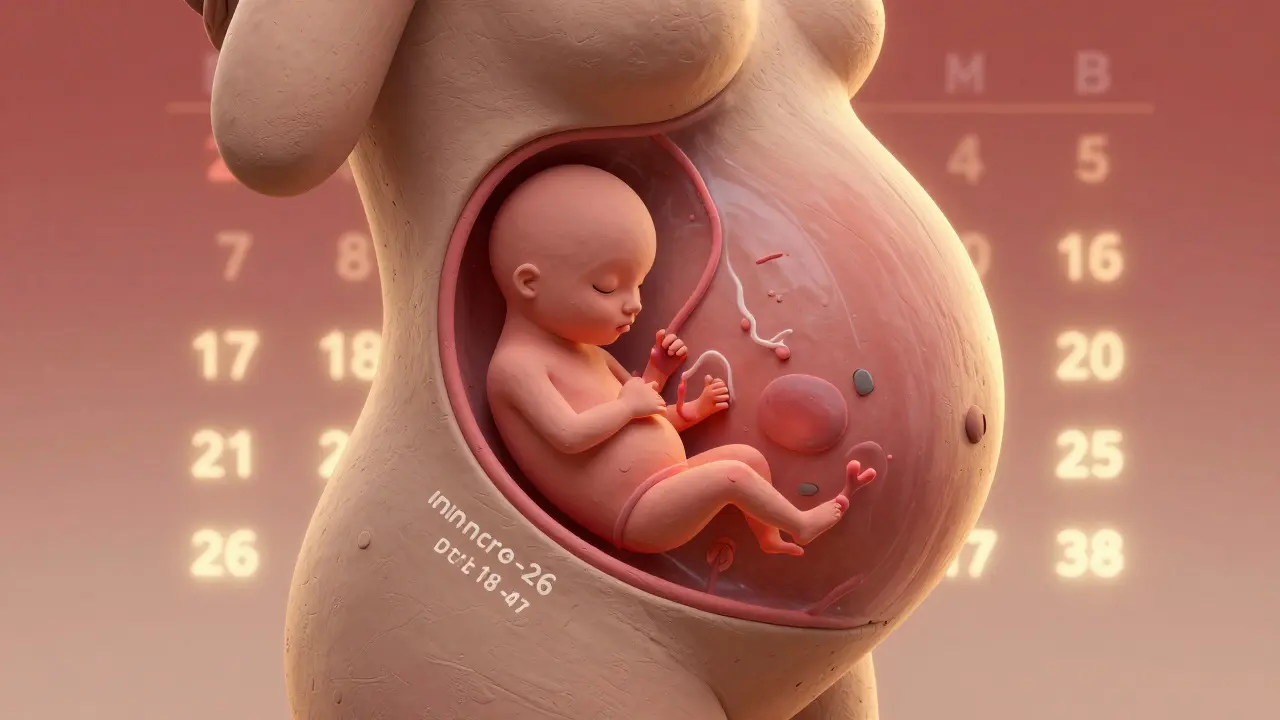
When you’re pregnant, every pill, drop, or spray you take matters more than ever. The first 12 weeks - known as the first trimester - are when your baby’s entire body is being built from scratch. This isn’t just a time of rapid growth. It’s a window of extreme vulnerability. Between days 17 and 56 after conception, even small exposures to certain medications can disrupt how organs form, leading to birth defects that last a lifetime.
The American College of Obstetricians and Gynecologists says 90% of major birth defects happen during this short window. That’s not a guess. It’s based on decades of tracking pregnancies and birth outcomes. Neural tubes close between days 18 and 26. The heart develops between days 20 and 40. Arms and legs take shape between days 24 and 36. Miss the timing, and the damage can be permanent.
What Medications Are Most Commonly Used - and Risky?
Most pregnant people take at least one medication in the first trimester. Some are prescribed. Others are bought over the counter. A study of over 5,000 pregnancies found that 30% of women took acetaminophen (Tylenol) for pain or fever. That’s more than one in three. It’s still considered the safest option, but new research shows even this common drug isn’t risk-free.
Long-term use of acetaminophen - more than a week or two - has been linked to a 30% higher chance of ADHD and a 20% higher chance of autism spectrum disorder in children. That doesn’t mean you can’t use it. It means you should use the lowest dose for the shortest time possible. If you’re taking it daily for headaches or back pain, talk to your provider. There might be other ways to manage it.
NSAIDs like ibuprofen (Advil) and naproxen (Aleve) are a different story. Even short-term use in the first trimester has been tied to a 1.6 times higher risk of miscarriage. The FDA warns that using these drugs after 20 weeks can cause serious kidney problems in the baby and reduce amniotic fluid. Avoid them entirely unless your doctor says otherwise.
Antidepressants and the Balancing Act
Untreated depression during pregnancy carries its own risks: preterm birth, low birth weight, and even long-term emotional challenges for the child. But some antidepressants carry known risks. Paroxetine (Paxil) has been linked to a 1.5 to 2 times higher chance of heart defects, especially ventricular septal defects. For that reason, many doctors avoid it in early pregnancy.
On the other hand, fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa) don’t show strong links to major birth defects. That doesn’t mean they’re perfect. They can cause neonatal adaptation syndrome - jitteriness, feeding trouble, breathing issues - in newborns if taken late in pregnancy. The key? Don’t stop your medication cold turkey. Work with your doctor to find the safest option and the lowest effective dose.

Antibiotics: Safe and Not So Safe
When you get a bacterial infection during pregnancy, antibiotics are often necessary. The good news? Many are safe. Amoxicillin, cephalosporins, and erythromycin are routinely used without evidence of harm. They’re considered low-risk and are often the first choice.
But some antibiotics are dangerous during this time. Tetracycline can permanently stain your baby’s teeth and affect bone growth - and that risk starts after week 15. Fluoroquinolones like ciprofloxacin damage cartilage in animal studies. Human data is limited, but most doctors avoid them entirely in pregnancy. Always tell your provider you’re pregnant before accepting any antibiotic.
What About Allergies, Colds, and Upset Stomach?
Pregnancy brings a lot of uncomfortable symptoms. Allergies, congestion, nausea - they’re common. But not all remedies are safe.
Diphenhydramine (Benadryl), loratadine (Claritin), and cetirizine (Zyrtec) are generally considered safe for allergies. But pseudoephedrine (Sudafed) should be avoided in the first trimester. One study found a 1.2 to 1.3 times higher risk of gastroschisis - a serious abdominal wall defect - in babies exposed to this decongestant early on.
For nausea, promethazine is sometimes prescribed, but it’s not the first-line choice anymore. Doxylamine combined with pyridoxine (Diclegis) is now preferred. It’s FDA-approved for pregnancy nausea and has a strong safety record.
For heartburn or stomach upset, avoid bismuth subsalicylate (Pepto-Bismol). It contains salicylates, which act like aspirin and carry risks. Loperamide (Imodium) has been linked to heart defects in one small study. H2 blockers like famotidine (Pepcid) are often used, but there’s not enough data to say they’re completely safe in the first trimester.
What About Chronic Conditions?
If you have epilepsy, diabetes, or an autoimmune disease, stopping your medication can be more dangerous than keeping it. Stopping seizure meds increases the risk of seizure-related fetal death by 400%. Uncontrolled diabetes raises the chance of major birth defects from 2-3% to 10-15%.
For thyroid disease, levothyroxine (Synthroid) is safe and often needs a higher dose during pregnancy. ACOG recommends keeping TSH under 2.5 mIU/L in the first trimester. For lupus or rheumatoid arthritis, hydroxychloroquine (Plaquenil) is considered safe and may even reduce flare-ups.
Corticosteroids like prednisone are trickier. One large study found a 1.3 to 1.6 times higher risk of cleft lip or palate with first-trimester use. But if you need them to control a serious condition, the benefits usually outweigh the risks. The goal is always the lowest dose for the shortest time.

What You Should Do - Step by Step
Here’s how to protect your baby and yourself:
- Confirm your dates. Know exactly when you conceived. Ultrasound dating is more accurate than your last period.
- Know your exposure window. If you took a medication between days 17 and 56 after conception, that’s the critical period.
- Don’t guess. Don’t rely on internet searches or well-meaning friends. Use trusted resources like MotherToBaby or TERIS (Teratology Information System).
- Try non-drug options first. For headaches, try cold compresses or rest. For nausea, ginger tea or acupressure bands help some women.
- Use the lowest dose for the shortest time. Even safe medications can have risks if overused.
- Keep a list. Write down every medication, supplement, and herb you take. Bring it to every appointment.
The Hard Truth: We Don’t Know Enough
Here’s the reality: 96% of medications used during pregnancy lack solid human data on fetal safety. The FDA says 98% of prescription labels don’t give clear pregnancy risk information. That’s not because doctors are careless. It’s because pharmaceutical companies rarely test drugs in pregnant people.
Dr. Christina Chambers from UC San Diego calls this a “prescription information desert.” Pregnant women are left guessing. That’s why services like MotherToBaby field over 15,000 calls a year from people asking, “Is this safe?”
Some progress is being made. The FDA’s Pregnancy Exposure Registry tracks outcomes for over 10,000 women exposed to specific drugs. PregSource, a research project that collected data from 12,000 pregnant people, is helping build better evidence. But until companies are required to study pregnancy safety, the gaps will remain.
Final Thoughts: Trust, But Verify
You’re not alone in feeling anxious. Nearly 70% of pregnant women take at least one medication. Over 40% have stopped a necessary drug because they were scared. That fear is real. But so is the risk of untreated illness.
The goal isn’t to avoid all medications. It’s to use the right ones, at the right time, in the right dose. Talk to your provider. Ask for evidence. Ask for alternatives. Ask what happens if you don’t treat this. You deserve clear answers - not silence.
When in doubt, call MotherToBaby. They’re free, confidential, and staffed by specialists who know exactly what’s safe and what’s not. You’re not just protecting your baby. You’re protecting your peace of mind.