When you pick up a prescription at the pharmacy, you might see a label that says generic - and wonder what that really means. But beyond just being a cheaper version of a brand-name drug, generics are organized into complex systems that doctors, pharmacists, and insurers use every day to make decisions about safety, cost, and effectiveness. Understanding how these drugs are classified isn’t just for experts - it helps you know why your doctor chose one drug over another, why your insurance covers one version but not another, and how the same pill can have different names depending on who’s talking about it.
Therapeutic Classification: What the Drug Treats
The most common way to group generic drugs is by what they’re used for - this is called therapeutic classification. Think of it like sorting tools by function: you don’t put a hammer in the screwdriver drawer, even if they’re both metal. Similarly, drugs are grouped by the medical condition they treat. A pain reliever goes in the analgesic category, a blood pressure pill goes in cardiovascular agents, and a thyroid hormone goes in endocrine agents.
The FDA and USP (United States Pharmacopeia) use a detailed system with over 300 therapeutic categories. For example, under Analgesics, you’ll find subgroups like Non-opioid Analgesics (think acetaminophen and ibuprofen) and Opioid Analgesics (like generic oxycodone). Under Antineoplastics, you’ll find chemotherapy drugs like methotrexate or 5-fluorouracil. Each category is further broken down into pharmacologic subclasses to help doctors choose the right drug for the right patient.
This system works well in hospitals and clinics because it’s practical. A nurse can quickly find all diabetes medications in one section. A pharmacist can check for duplicates. But it has a flaw: some drugs do more than one thing. Aspirin, for example, reduces pain, prevents blood clots, and lowers inflammation. Should it be in analgesics, anticoagulants, or anti-inflammatories? Therapeutic classification forces a choice - and that’s where confusion starts.
Pharmacological Classification: How the Drug Works
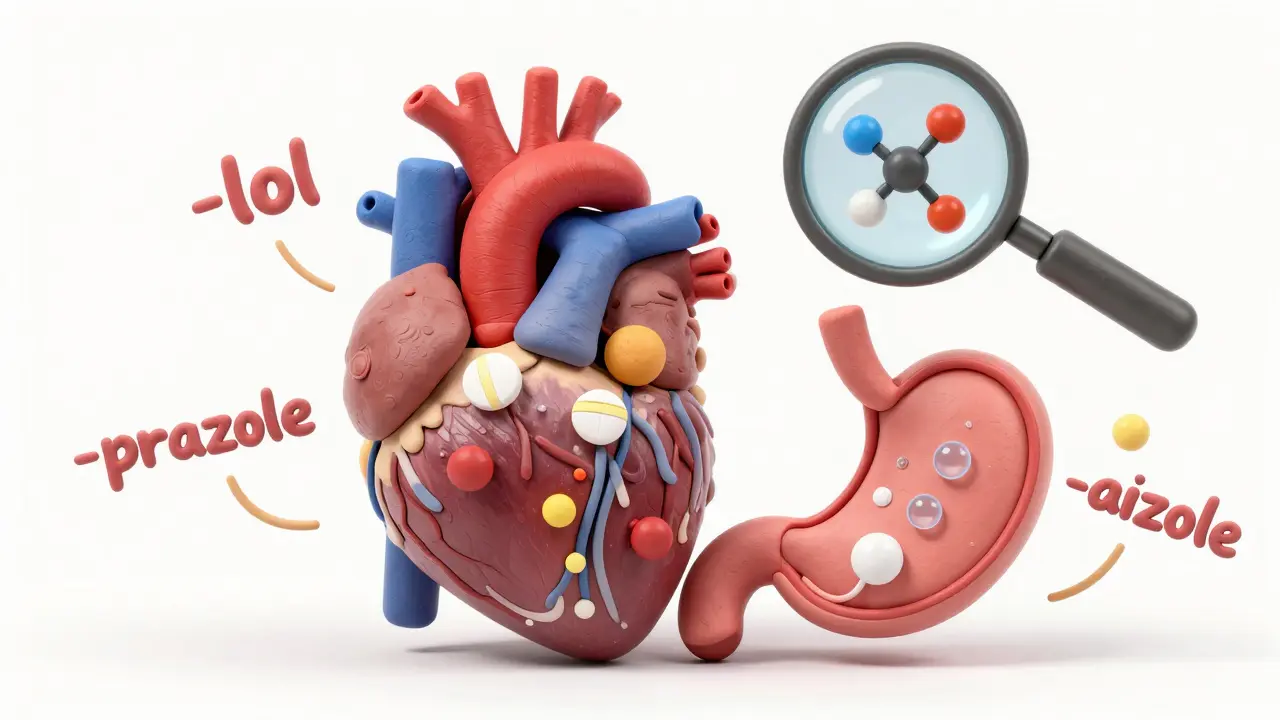
If therapeutic classification asks, “What does it treat?”, pharmacological classification asks, “How does it work?” This system looks at the drug’s biological mechanism - the exact molecular interaction that changes how your body behaves.
For instance, drugs ending in -lol - like metoprolol or atenolol - are all beta-blockers. They work by blocking adrenaline receptors in the heart, slowing heart rate and lowering blood pressure. Drugs ending in -prazole - like omeprazole or esomeprazole - are proton pump inhibitors. They shut down acid production in the stomach. These naming patterns aren’t random; they’re part of a formal system called stem nomenclature, adopted by the USP in 1964 and still updated every year.
There are about 1,200 distinct pharmacologic classes identified in current medical literature. Some are very specific: Epidermal Growth Factor Receptor Kinase Inhibitors (used in lung cancer) or Purine Analogs (used in leukemia). These are powerful for researchers and oncologists because they reveal how drugs target disease at the cellular level. But they’re not useful for a busy family doctor trying to decide between two generic antidepressants. The science is precise - but too technical for daily use.
DEA Schedules: Legal Status and Abuse Risk
Not all drugs are treated the same under the law. The Drug Enforcement Administration (DEA) classifies controlled substances into five schedules based on two factors: how likely they are to be abused, and whether they have accepted medical uses.
- Schedule I: No medical use, high abuse potential - examples: heroin, LSD, marijuana (still federally classified this way, despite state laws).
- Schedule II: High abuse potential, but medical use - examples: oxycodone, fentanyl, Adderall.
- Schedule III: Moderate abuse potential, accepted medical use - examples: hydrocodone with acetaminophen, ketamine, buprenorphine.
- Schedule IV: Low abuse potential - examples: alprazolam (Xanax), diazepam (Valium), zolpidem (Ambien).
- Schedule V: Very low abuse potential - examples: cough syrups with small amounts of codeine (under 200mg per 100ml).
This system affects prescriptions. Schedule II drugs can’t be refilled without a new prescription. They require special paperwork. Pharmacies must store them separately. But here’s the problem: the DEA system doesn’t care about how well a drug works - only about abuse risk. That’s why oxycodone (Schedule II) causes more overdose deaths than heroin (Schedule I) - but heroin is considered “worse” under the law. Critics say this disconnect makes the system outdated, especially as medical science evolves.
Insurance Tiers: What You Pay Out of Pocket
Your insurance plan doesn’t care about therapeutic groups or molecular mechanisms. It cares about cost. That’s why most plans use a tier system - usually five levels - to decide how much you pay for each drug.
- Tier 1: Preferred generics - lowest cost. These are the most commonly prescribed and cheapest options. About 75% of all generic drugs fall here.
- Tier 2: Non-preferred generics - slightly more expensive, often because the insurer has a deal with a different brand.
- Tier 3: Preferred brand-name drugs - you pay more than for generics, but less than non-preferred brands.
- Tier 4: Non-preferred brand-name drugs - high cost, usually because cheaper alternatives exist.
- Tier 5: Specialty drugs - expensive, complex medications (like biologics for rheumatoid arthritis or cancer). These make up just 5-7% of prescriptions but account for nearly half of total drug spending.
Here’s the kicker: two identical generic drugs - same active ingredient, same dosage, same manufacturer - can end up in different tiers based on which company struck a deal with your insurer. A 30-day supply of generic lisinopril might cost $4 in Tier 1, but $12 in Tier 2 - even though they’re chemically the same. This frustrates patients and pharmacists alike. In fact, 43% of prior authorization requests from pharmacies are due to tier disputes, according to pharmacist forums.
The ATC System: The Global Standard
While the U.S. uses multiple overlapping systems, the World Health Organization (WHO) created a single global standard: the Anatomical Therapeutic Chemical (ATC) classification. It’s used in 143 countries and forms the backbone of drug statistics worldwide.
The ATC system has five levels:
- Level 1: Anatomical main group (e.g., A = Alimentary tract and metabolism, C = Cardiovascular system)
- Level 2: Therapeutic subgroup (e.g., C03 = Diuretics)
- Level 3: Pharmacological subgroup (e.g., C03A = High-ceiling diuretics)
- Level 4: Chemical subgroup (e.g., C03CA = Sulfonamides)
- Level 5: Chemical substance (e.g., C03CA01 = Furosemide)
So furosemide - a loop diuretic - gets the code C03CA01. This level of detail lets researchers track usage patterns across countries, compare prescribing habits, and spot emerging trends. The WHO adds about 200 new ATC codes every year as new drugs enter the market. It’s the most complete system available - but it’s not used in daily clinical practice in the U.S. Instead, it’s mostly used for research, public health reporting, and global drug monitoring.

Why Classification Confusion Costs Time and Money
Healthcare workers don’t use just one system - they juggle all of them. A doctor chooses a drug based on therapeutic use. A pharmacist checks the DEA schedule to know how to dispense it. A billing clerk looks up the insurance tier to figure out patient cost. An EHR system pulls in ATC codes for reporting. And if any of these don’t match up, errors happen.
Studies show that 27% of medication errors in hospitals are tied to classification confusion. A nurse might grab the wrong generic because two drugs look similar on the shelf - one is in Tier 1, the other Tier 2, but both are labeled “generic metoprolol.” A physician might prescribe a Schedule III drug thinking it’s safe to refill - not realizing it’s still tightly controlled. Patients get confused when their insurance denies coverage for a drug they’ve been taking for years - because it was moved from Tier 1 to Tier 2.
A 2022 survey by the American Medical Association found that primary care doctors spend 12 to 18 minutes per patient just navigating these conflicting systems. Family practitioners reported 23% higher confusion rates than specialists. That’s not just frustrating - it’s dangerous.
What’s Changing in 2025 and Beyond
Classification systems are starting to evolve. In September 2023, the FDA announced its Therapeutic Categories Model 2.0, launching in January 2025. This new version allows drugs to have a primary and secondary therapeutic indication. So aspirin can now be listed as both an analgesic and an antiplatelet agent - no more forced choices.
Meanwhile, the WHO is preparing its 2024 ATC update to include 32 new biologic drugs - like cell therapies and monoclonal antibodies - which don’t fit neatly into old chemical categories. And AI tools like IBM Watson’s Drug Insight platform are being tested to predict the best classification for new drugs with 92.7% accuracy.
But the biggest change may come from policy. The MORE Act, passed by the House in 2023, could reclassify marijuana from Schedule I to Schedule III. If it becomes law, it would force a cascade of updates across DEA records, insurance formularies, and hospital databases - all because one classification changed.
One thing is clear: as drugs get more complex - with multiple uses, targeted mechanisms, and personalized effects - our old ways of sorting them are breaking down. The future will need systems that are flexible, digital, and integrated. Until then, understanding these five classification layers - therapeutic, pharmacological, legal, insurance, and global - gives you the power to ask better questions, understand your prescriptions, and navigate the system with more confidence.
What’s the difference between therapeutic and pharmacological classification?
Therapeutic classification groups drugs by the medical condition they treat - like pain, high blood pressure, or depression. Pharmacological classification groups them by how they work at the molecular level - like blocking beta receptors or inhibiting acid production. One tells you what it does for you; the other tells you how it does it.
Why is my generic drug in a higher insurance tier than another generic?
Even if two generic drugs have the same active ingredient, your insurance plan may prefer one manufacturer over another due to pricing deals. The higher-tier drug isn’t stronger or better - it’s just more expensive for your plan to cover. You can ask your pharmacist to check if a lower-tier alternative is available.
Are all generic drugs the same as brand-name drugs?
Yes - by law, the FDA requires generics to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also be bioequivalent, meaning they work the same way in your body. The only differences are in inactive ingredients like fillers or dyes - which rarely affect how the drug works.
Why is marijuana still a Schedule I drug if it’s legal in many states?
Marijuana is classified as Schedule I at the federal level because the DEA still considers it to have no accepted medical use and high abuse potential. But 38 states allow medical use, and the FDA has approved cannabinoid-based medications like dronabinol (Schedule II). This federal-state conflict creates legal and prescribing confusion, and many experts argue the classification is outdated.
Do drug classification systems affect how I get my medication?
Absolutely. Your doctor’s choice of drug may be limited by insurance tiers. Your pharmacy may need special paperwork if the drug is DEA-controlled. And if your drug is misclassified in your electronic health record, it could be flagged as a duplicate or denied coverage. Understanding these systems helps you advocate for yourself - like asking for a tier exception or checking if a generic alternative exists.

