When your stomach hurts, you’re bloated, and you’re running to the bathroom constantly, it’s easy to assume it’s just food poisoning or stress. But for millions of people, these symptoms don’t go away. They’re signs of something deeper: inflammatory bowel disease, or IBD. Two main conditions fall under this umbrella - Crohn’s disease and ulcerative colitis. They sound similar, share symptoms, and even get mixed up by doctors sometimes. But they’re not the same. And knowing the difference isn’t just academic - it changes everything about how you live, what treatments work, and what complications you might face.
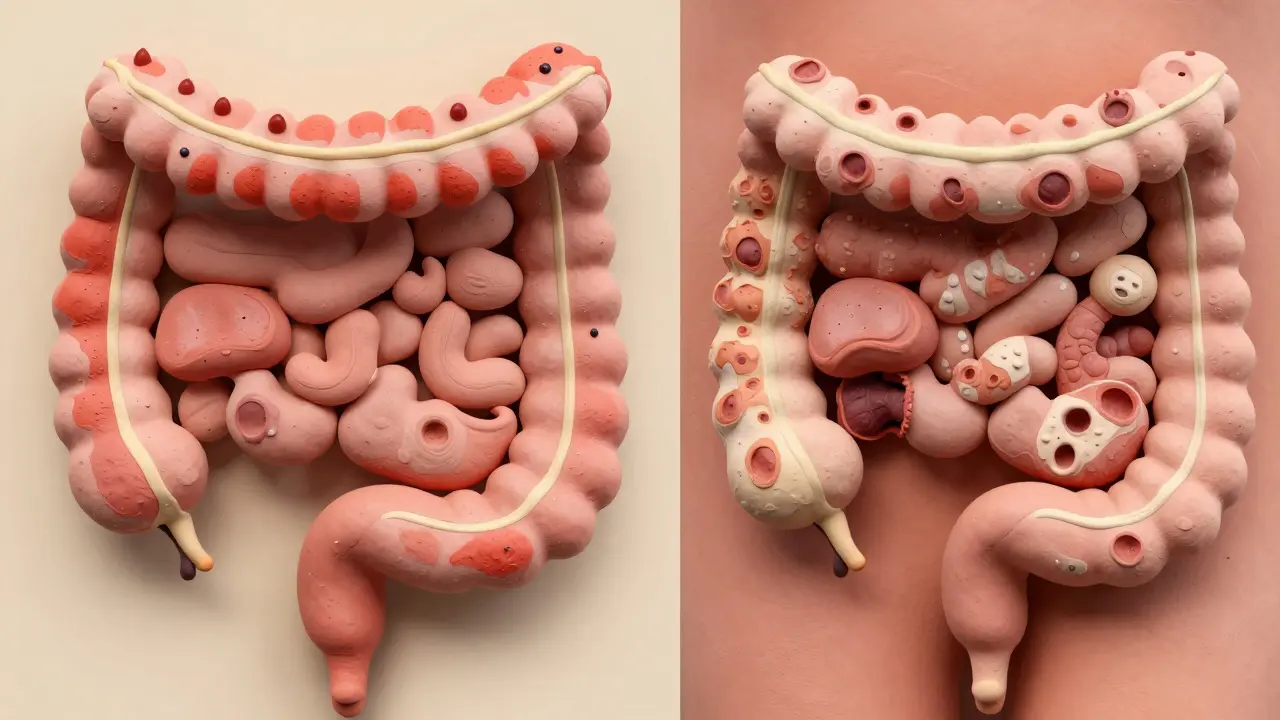
Where the Inflammation Happens
- Ulcerative colitis (UC) only hits the colon and rectum - the last part of your digestive tract. The inflammation starts at the rectum and creeps upward in a continuous line. There are no gaps. If you look at the colon with a scope, you’ll see red, raw, bleeding tissue from the bottom all the way up to where it stops.
- Crohn’s disease? It can show up anywhere. Mouth to anus. It most often hits the end of the small intestine (ileum) and the beginning of the colon, but it doesn’t care where it lands. And here’s the big clue: it doesn’t spread in a line. It skips. Healthy patches of tissue sit between inflamed ones. That’s called "skip lesions," and it’s a dead giveaway for Crohn’s.
This difference isn’t just about location. It’s about depth. Ulcerative colitis sticks to the innermost layer - the mucosa. Think of it like a sunburn on the surface. Crohn’s, though, digs all the way through. It punches through the muscle layers, sometimes even breaking out into nearby organs. That’s why Crohn’s patients are at risk for fistulas - abnormal tunnels between the bowel and bladder, skin, or other intestines. You don’t see that with UC.
What the Inside Looks Like
During a colonoscopy, doctors look for clues. In ulcerative colitis, the lining looks uniformly inflamed. You’ll often see pseudopolyps - little bumps of healing tissue rising up from the damaged surface. In Crohn’s, the lining looks like cobblestones. Deep cracks and ulcers form between raised areas. It’s like the surface has cracked open and never fully healed.
Biopsies confirm it. UC shows inflammation only in the top layers. Crohn’s shows granulomas - clusters of immune cells that form when the body tries to wall off something it can’t get rid of. These aren’t always present, but when they are, they’re almost always Crohn’s.
Complications Are Different
Both conditions can make you tired, cause weight loss, and lead to bloody diarrhea. But the risks diverge sharply.
- Crohn’s patients have a 1 in 3 chance of developing strictures - scar tissue that narrows the bowel. That can block food and waste. About 1 in 4 will get fistulas. These are painful, can get infected, and often need surgery.
- Ulcerative colitis rarely causes strictures or fistulas. But it carries a different threat: toxic megacolon. During a severe flare, the colon can suddenly swell and balloon out. It’s rare - under 5% of UC cases - but it’s life-threatening. The colon can rupture. That’s an emergency.
Both can cause problems outside the gut. Joint pain, skin rashes, eye inflammation - these affect about a third of IBD patients. But one condition has a strong link to liver disease: primary sclerosing cholangitis (PSC). It’s found in 3-7% of UC patients but less than 1% of Crohn’s patients. If you have UC and your liver enzymes are off, this is something your doctor needs to check.
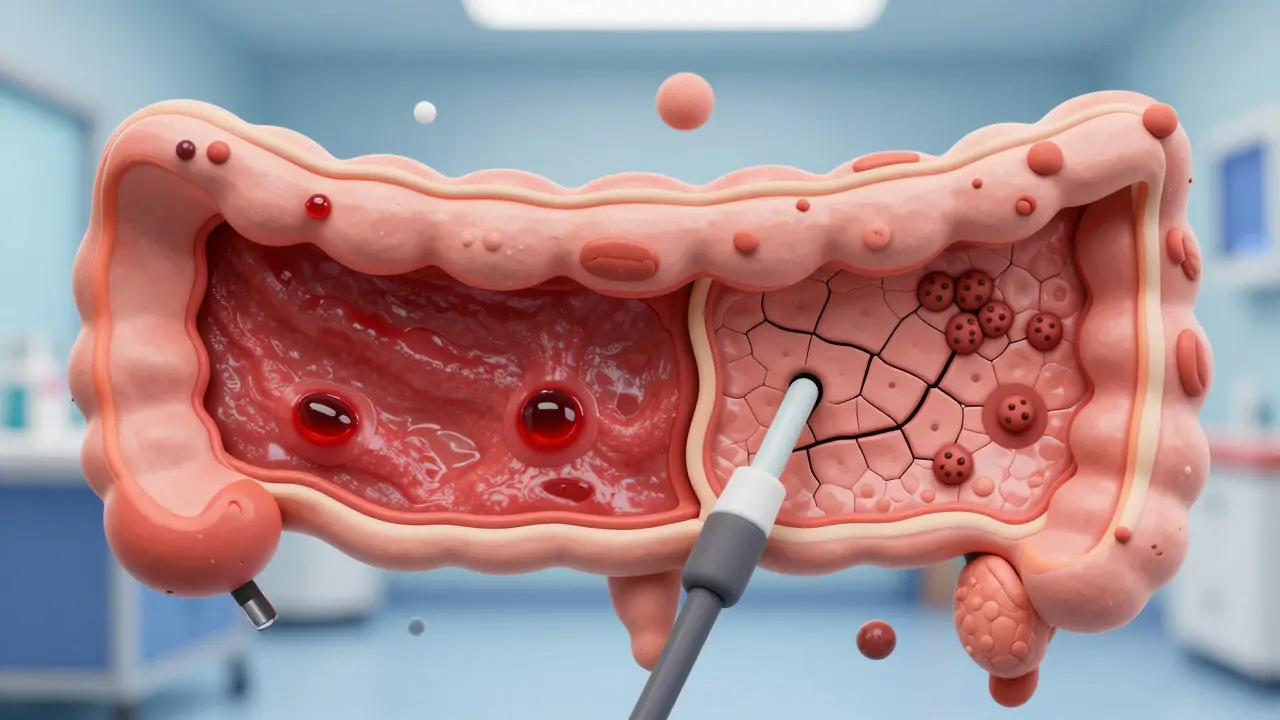
How They’re Diagnosed
There’s no single blood test that says "Crohn’s" or "UC." Diagnosis is like putting together a puzzle. You need symptoms, scans, endoscopy, and biopsies.
- Colonoscopy with biopsy is the gold standard. For UC, the pattern is clear: continuous inflammation starting at the rectum. For Crohn’s, skip lesions and transmural damage are the clues.
- Imaging helps. MRI enterography or CT scans can show thickening of the bowel wall - common in Crohn’s. Capsule endoscopy (swallowing a tiny camera) finds small bowel damage that colonoscopes miss. That’s almost always Crohn’s.
- Blood and stool tests give hints. Fecal calprotectin is high in both, but it’s usually higher in UC. A blood test for pANCA (anti-neutrophil cytoplasmic antibodies) is positive in 60-70% of UC patients but only 10-15% of Crohn’s patients. It’s not perfect, but it helps.
And here’s something most people don’t know: about 10-15% of cases start as "indeterminate colitis." The signs don’t clearly point to either Crohn’s or UC. Doctors watch and wait. Sometimes, years later, new symptoms or complications reveal the true diagnosis.
Treatment Isn’t One-Size-Fits-All
Both conditions use similar drugs - anti-inflammatories, immunosuppressants, biologics - but how they’re used differs.
- For mild to moderate UC, enemas and suppositories with 5-ASAs (like mesalamine) work wonders. They deliver the drug right where it’s needed - the colon. Up to 80% of patients respond well.
- Crohn’s needs systemic treatment. Pills or injections that reach the whole gut. Azathioprine or methotrexate are common. Biologics like infliximab or adalimumab help about 30-40% of Crohn’s patients achieve remission, compared to 20-30% in UC.
Surgery is where the biggest difference lies.
- For ulcerative colitis, removing the entire colon and rectum is a cure. After surgery, many patients get an ileal pouch - a new internal reservoir made from the small intestine. They can still pass stool normally. About 10-15% of UC patients eventually need this.
- Crohn’s surgery? It’s not a cure. Surgeons remove the damaged section, but the disease always comes back - often right next to the scar. Half of Crohn’s patients need another surgery within 10 years. That’s why doctors try to avoid surgery if they can.

Life With IBD: What Patients Say
Real people, real experiences. In online communities, UC patients talk more about urgency - that sudden, uncontrollable need to go. About 87% report it as their biggest issue. Rectal bleeding? That’s common too - 75% of UC patients see blood in their stool.
Crohn’s patients? They worry more about nutrition. If your small intestine is inflamed, you can’t absorb vitamins, iron, or calories. Weight loss, anemia, and fatigue are daily battles. One in two Crohn’s patients say food triggers their flares - dairy, fiber, fried stuff. Stress hits both groups, but UC patients name it as the top trigger in over 60% of posts.
Costs and Future Hope
IBD is expensive. Severe Crohn’s costs nearly $40,000 a year in medical care. Severe UC isn’t far behind - around $38,000. That’s not just drugs - it’s hospital stays, scans, lost work days.
But new treatments are coming. Fecal microbiota transplants (FMT) - basically, poop from a healthy donor - showed 32% remission in UC patients in a 2022 trial. For Crohn’s? Only 22%. That tells us the gut microbiome plays different roles in each disease.
Drugs like mirikizumab (for Crohn’s) and etrolizumab (for UC) are in final testing. FDA decisions are expected by late 2024. These target specific immune pathways, offering hope for better control with fewer side effects.
Bottom Line
Crohn’s disease and ulcerative colitis aren’t just two names for the same thing. They’re different diseases with different patterns, risks, and treatments. One is a surface burn; the other is a deep, unpredictable fire. One can be cured by removing the colon; the other will keep coming back, no matter how much you cut out.
If you’re living with IBD, knowing which one you have isn’t about labels. It’s about survival. It’s about choosing the right meds, avoiding the right complications, and planning your life around what your body can handle. And if you’re still unsure? Don’t rush. Sometimes, it takes years to know for sure. Watch. Listen. Track your symptoms. Your body will tell you - if you’re paying attention.
Can you have both Crohn’s disease and ulcerative colitis at the same time?
No, you can’t have both at the same time. They are two distinct conditions. But about 10-15% of cases start as "indeterminate colitis," where doctors can’t tell which one it is right away. Over time, as symptoms or complications develop, the diagnosis usually becomes clearer. Some people initially diagnosed with UC later turn out to have Crohn’s - especially if they develop fistulas or skip lesions.
Does stress cause IBD?
Stress doesn’t cause Crohn’s or ulcerative colitis. These are autoimmune conditions triggered by genetics and immune system misfires, not by anxiety or pressure. But stress can absolutely make flares worse. Many patients report that high-stress periods - job loss, divorce, illness - lead to more frequent or severe symptoms. Managing stress doesn’t cure IBD, but it helps you stay in remission longer.
Is IBD the same as IBS?
No, they’re completely different. IBS - irritable bowel syndrome - is a functional disorder. The gut looks normal on scans and biopsies, but it doesn’t work right. Symptoms include bloating, cramping, and changes in bowel habits, but there’s no inflammation or tissue damage. IBD involves real, visible inflammation that can destroy the bowel lining. IBS doesn’t lead to cancer or need surgery. IBD can.
Can diet cure IBD?
No diet can cure Crohn’s or ulcerative colitis. But what you eat can help manage symptoms. Some people find that avoiding dairy, spicy foods, or high-fiber items reduces flares. Others benefit from low-FODMAP diets or exclusive enteral nutrition (a liquid diet) for Crohn’s. These don’t fix the immune problem, but they can give your gut a break and improve quality of life. Always work with a dietitian who knows IBD - not just any nutritionist.
Will I need surgery?
For ulcerative colitis, surgery is a real possibility - about 1 in 10 people will need their colon removed at some point. It’s often curative. For Crohn’s, surgery is common - up to half of patients need it within 10 years - but it’s not a cure. The disease comes back, often near the surgical site. Doctors avoid surgery for Crohn’s if possible, because it doesn’t solve the problem, just moves it.
Are these conditions hereditary?
Yes, genetics play a role. If you have a first-degree relative (parent, sibling, child) with IBD, your risk is 5-10 times higher than the general population. But having the genes doesn’t mean you’ll get it. Environmental factors - like smoking, antibiotics, diet, and where you live - also matter. Many people with IBD have no family history at all.
Can IBD lead to cancer?
Yes, especially with long-standing ulcerative colitis. If you’ve had inflammation in your colon for more than 8-10 years, your risk of colon cancer goes up. That’s why regular colonoscopies with biopsies are recommended every 1-2 years after that point. Crohn’s disease involving the colon also increases risk, but less so than UC. Managing inflammation with medication reduces this risk significantly.