What Counts as a Severe Drug Reaction?
A severe adverse drug reaction isn’t just a rash or an upset stomach. It’s when your body turns against a medication you took-sometimes within minutes, sometimes after weeks-and starts shutting down vital systems. The difference between a mild reaction and a life-threatening one is often just minutes. According to the U.S. Food and Drug Administration, a serious adverse event means the reaction caused death, was life-threatening, required hospitalization, led to permanent damage, or disrupted normal body function in a way that demands urgent care.
Three drugs stand out as the most dangerous when things go wrong: blood thinners like warfarin, diabetes medications like insulin, and opioids like morphine. These aren’t rare drugs-they’re prescribed daily. But when they trigger a severe reaction, the results can be fatal. For example, a single wrong dose of insulin can drop blood sugar so low it causes seizures or coma. An overdose of an opioid can stop your breathing entirely. And a blood thinner can cause internal bleeding you don’t even feel until it’s too late.
Signs You’re Having a Life-Threatening Reaction
Knowing the warning signs can save your life-or someone else’s. Here’s what to watch for:
- Difficulty breathing or wheezing-this isn’t just a cold. If you feel like you can’t get air in, even when sitting still, it’s an emergency.
- Swelling of the face, lips, tongue, or throat-this can block your airway in minutes. You might notice your voice getting hoarse or your tongue feels thick.
- Sudden dizziness, fainting, or rapid heartbeat-your body is going into shock. Blood pressure drops fast, and your heart tries to compensate.
- A widespread rash with blisters or peeling skin-especially if it’s spreading fast. If more than 10% of your skin starts peeling off, you could be developing Toxic Epidermal Necrolysis (TEN), a condition with a 30-50% death rate.
- Fever, sore throat, or mouth sores-paired with a rash, this could signal DRESS syndrome, which attacks your organs.
These symptoms don’t always show up right away. Some reactions hit within 10 minutes of taking a pill. Others take days or even weeks. That’s why you can’t ignore a new rash or fever just because you took the drug a week ago.
Anaphylaxis: The Silent Killer
Anaphylaxis is the most dangerous type of drug reaction. It’s an all-out immune system meltdown triggered by things like antibiotics, NSAIDs, or even contrast dye used in CT scans. It doesn’t care if you’ve taken the drug before without issue. One time it’s fine. The next, your body goes into overdrive.
The signs are fast and brutal: hives, swelling, coughing, vomiting, and a sudden drop in blood pressure. Without treatment, death can happen in under an hour. The Resuscitation Council UK says you shouldn’t wait for a doctor to confirm it. If you see even two of these symptoms-trouble breathing and swelling, for example-give epinephrine immediately.
Epinephrine is not optional. It’s the only thing that can reverse the process. It’s injected into the thigh, not the arm. The dose is 0.01 mg per kilogram of body weight-most auto-injectors deliver 0.3 mg or 0.5 mg, which is safe for adults. If symptoms don’t improve in 5 to 15 minutes, give a second dose. Don’t wait for an ambulance. Don’t try antihistamines first. Epinephrine comes first. Always.

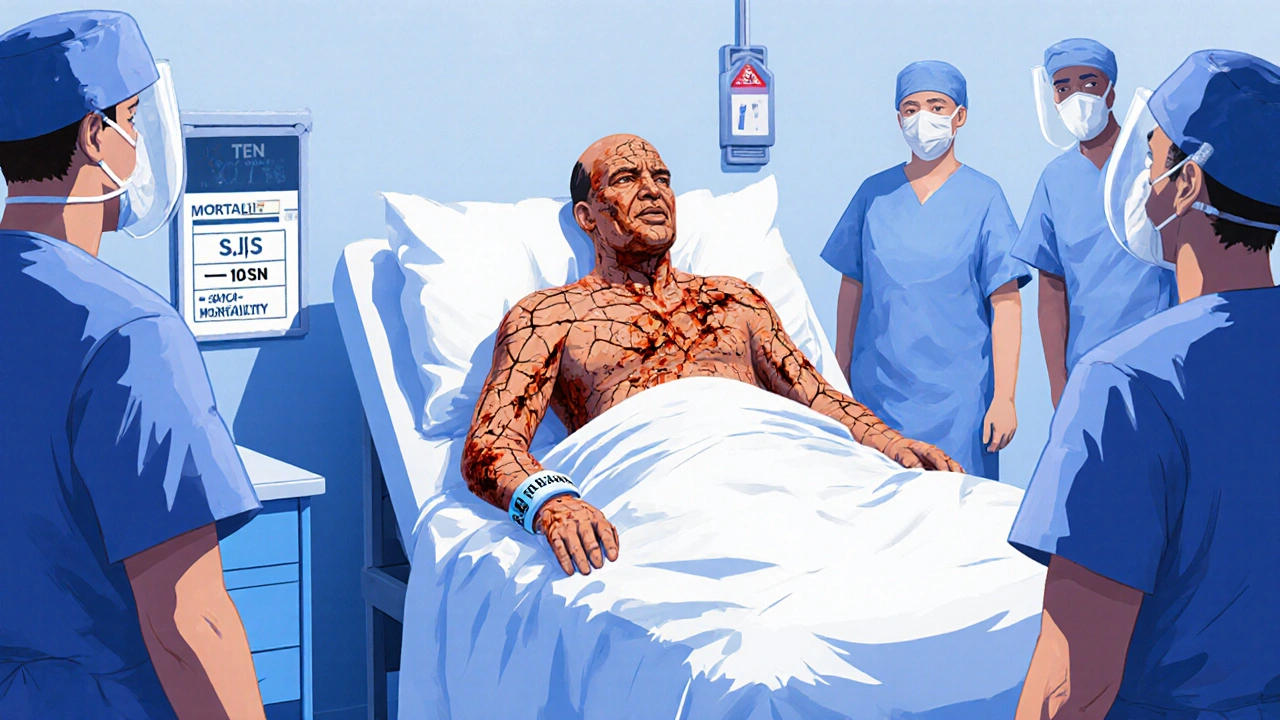
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: Skin That Starts to Die
These are rare but devastating reactions. You might start with flu-like symptoms-fever, sore throat, burning eyes. Then, a red or purplish rash spreads. Blisters form. Within days, your skin begins to detach, like a severe burn. This is Stevens-Johnson Syndrome (SJS) if less than 10% of your skin is affected. If more than 30% peels off, it’s Toxic Epidermal Necrolysis (TEN). The mortality rate for TEN is as high as 50%.
Drugs that commonly cause this include allopurinol (used for gout), sulfonamide antibiotics, seizure medications like carbamazepine, and some painkillers. It usually shows up 1 to 3 weeks after starting the drug. If you notice your skin sloughing off in sheets, or if your mouth, eyes, or genitals are covered in blisters, get to a hospital immediately. This isn’t a dermatologist visit. This is a burn unit emergency. You’ll need intensive care, IV fluids, and specialists who know how to treat skin loss.
What to Do Right Now: A Step-by-Step Emergency Plan
If you or someone else is showing signs of a severe drug reaction, here’s exactly what to do:
- Stop the drug immediately. Don’t wait to see if it gets better. Take it away from them.
- Call 911 or your local emergency number. Say: “I think this is a severe drug reaction-possible anaphylaxis or skin detachment.”
- If epinephrine is available, use it now. Inject into the outer thigh. Even if you’re unsure, use it. It’s safe. The risk of not using it is death.
- Keep the person lying down. Elevate their legs if they’re dizzy. If they’re having trouble breathing, let them sit up.
- Don’t give them anything to eat or drink. Swelling in the throat can make swallowing dangerous.
- Bring the medication bottle with you to the hospital. This helps doctors identify the culprit fast.
Never try to “wait it out.” Severe reactions don’t get better on their own. Delaying care increases the chance of permanent damage or death.
Who Should Carry Epinephrine?
If you’ve ever had a severe allergic reaction to a drug, you should carry an epinephrine auto-injector-always. That includes people who’ve had anaphylaxis from penicillin, NSAIDs, or even vaccines. The American Academy of Family Physicians says anyone with a history of severe drug allergy should have two injectors on hand at all times. They should also have a written emergency action plan and know how to use the device.
Training matters. Many people own epinephrine but don’t know how to use it correctly. Some inject it into the wrong spot. Others hesitate because they’re afraid of the needle. Practice with a trainer device. Show your family how to use it. Make sure your kids, coworkers, or roommates know where it is and what to do.
Reporting Reactions Helps Save Lives
Every time a severe reaction happens, it should be reported-not just to your doctor, but to the FDA through their MedWatch program. These reports help regulators spot dangerous drugs before more people get hurt. In 2022, over 20 million suspected drug reactions were reported globally through the WHO’s monitoring system. Many of these were preventable.
When you report a reaction, you’re not just protecting yourself. You’re helping future patients avoid the same danger. Hospitals and pharmacies also track these events. If your doctor knows you had a reaction to a certain drug, they won’t prescribe it again.
What Happens After the Emergency?
Surviving a severe reaction doesn’t mean the danger is over. You’ll need follow-up care with an allergist or immunologist. They’ll do tests to confirm what caused it-skin tests, blood tests, or even controlled drug challenges in a safe setting.
You’ll get a medical alert bracelet or card listing your drug allergies. You’ll be given a personalized emergency plan. And you’ll learn which drugs to avoid forever. Some reactions mean you can never take another drug in the same class. For example, if you had SJS from sulfamethoxazole, you’ll likely need to avoid all sulfa drugs for life.
Final Warning: Don’t Assume It’s Just a Rash
Too many people brush off a new rash or mild swelling because “it’s probably nothing.” But with drug reactions, “nothing” can turn into death in under an hour. If you’re unsure, err on the side of caution. Use epinephrine. Call 911. Get to a hospital. Your life isn’t worth the gamble.
Can a drug reaction happen even if I’ve taken the medicine before without problems?
Yes. Your immune system can change over time. A drug that was safe last year can trigger a severe reaction this year. That’s why you should never assume you’re immune to side effects just because you’ve used the drug before.
Is it safe to take antihistamines like Benadryl instead of epinephrine during an allergic reaction?
No. Antihistamines can help with mild itching or hives, but they do nothing to stop the life-threatening drop in blood pressure or airway swelling caused by anaphylaxis. Epinephrine is the only treatment that reverses these effects. Delaying epinephrine to take antihistamines first increases the risk of death.
How long after taking a drug can a severe reaction occur?
It varies. Anaphylaxis usually happens within minutes to 2 hours. Skin reactions like SJS or DRESS can take days to weeks. Some reactions, like blood cell disorders from chemotherapy, can show up months later. Always monitor for new symptoms after starting any new medication-even if you’ve taken it before.
Can I get tested to find out which drugs I’m allergic to?
Yes, but only after a severe reaction. Allergists use skin tests or blood tests to confirm IgE-mediated allergies like penicillin. For reactions like SJS or DRESS, there’s no reliable test-you’re diagnosed based on symptoms and timing. Avoiding the drug and similar ones is the only sure protection.
Are over-the-counter drugs like ibuprofen or aspirin dangerous?
Yes. Even common OTC drugs can trigger severe reactions. Ibuprofen and aspirin have caused anaphylaxis in people with asthma or nasal polyps. Aspirin can also cause a rare but deadly skin reaction called SJS. Never assume a drug is safe just because it’s available without a prescription.
What should I do if I witness someone having a severe drug reaction?
Call 911 immediately. Ask if they have an epinephrine auto-injector. If yes, help them use it or use it for them if they’re unable. Keep them lying down, loosen tight clothing, and stay with them until help arrives. Don’t give them food, drink, or other medications. Your quick action can save their life.

