Omega-3 Dose Calculator for Colitis
Dosing Guide
Based on clinical evidence for colitis management
- Therapeutic range 2-4 g/day EPA/DHA
- Preferred source EPA-rich fish oil
- Take with meals For better absorption
Your Omega-3 Dosage Calculator
Your Recommended Dose
Based on clinical evidence for colitis management
Key Takeaways
- Omega-3 fatty acids modulate inflammation pathways that drive colitis symptoms.
- Clinical evidence points to EPA‑rich fish oil as the most effective form for reducing flare‑ups.
- Typical therapeutic doses range from 2 to 4g of combined EPA/DHA per day, taken with meals.
- Plant‑based ALA sources can complement fish oil but need conversion to EPA/DHA, which is limited.
- Potential side‑effects are mild but include gastrointestinal upset and increased bleeding risk at high doses.
When you hear the term Omega-3 fatty acids, you probably think of salmon, walnuts, or the little capsules people pop after meals. But what does that have to do with colitis - a chronic inflammation of the colon that can wreck daily life? The answer lies in how these fats talk to the immune system, the gut lining, and the tiny microbes that call your intestines home.
Omega-3 fatty acids are a family of polyunsaturated fats that include eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha‑linolenic acid (ALA). They are called "essential" because the body cannot make them from scratch; you must obtain them from food or supplements. In the context of colitis, EPA and DHA are the star players, while ALA - found in flaxseed, chia, and walnuts - serves as a modest backup that the body can only partially convert.
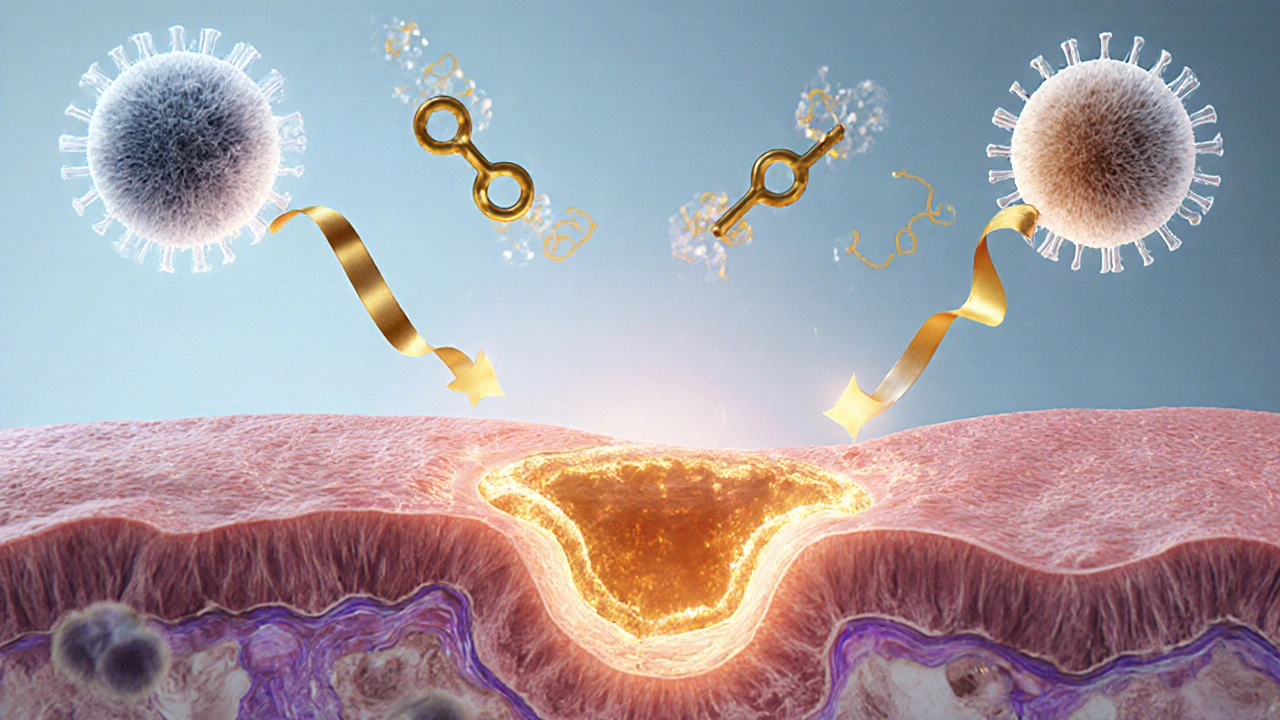
Why Inflammation is the Core Problem in Colitis
Colitis is a type of inflammatory bowel disease (IBD) that causes the inner lining of the colon to become inflamed, ulcerated, and leaky. The immune system mistakenly attacks the gut wall, releasing pro‑inflammatory cytokines such as tumor necrosis factor‑alpha (TNF‑α), interleukin‑1β (IL‑1β), and interleukin‑6 (IL‑6). These messengers recruit white blood cells, widen the blood vessels, and amplify pain, diarrhea, and bleeding.
Breaking this cycle requires either dampening the cytokine storm or strengthening the barrier that keeps harmful bacteria out. Omega‑3s influence both pathways.
How Omega‑3s Tame the Immune Fire
EPA and DHA are converted inside the body into specialized pro‑resolving mediators (SPMs) such as resolvins, protectins, and maresins. These SPMs act like peacekeepers: they signal immune cells to stop releasing TNF‑α and IL‑6, encourage clearance of dead cells, and promote tissue repair.
Scientific studies have mapped the chain of events with clear semantic triples:
- EPA is converted into resolvinE1.
- ResolvinE1 reduces neutrophil infiltration in the colon.
- DHA produces protectinD1, which enhances epithelial barrier function.
When these mediators are plentiful, the gut’s inflammatory response wanes, leading to fewer symptoms and longer remission periods.
What the Evidence Says - Clinical Trials and Real‑World Data
Multiple randomized controlled trials (RCTs) published between 2015 and 2024 have examined fish‑oil supplementation in ulcerative colitis (UC) and Crohn’s disease, the two main forms of IBD. A meta‑analysis of eight RCTs (total n≈1,200) found that participants taking ≥2g EPA/DHA daily experienced a 30% reduction in clinical relapse rates compared with placebo.
Key trial snapshots:
- German Study 2021: 120 UC patients received 3g EPA/DHA for 12weeks. Endoscopic scores improved in 68% of the supplement group versus 34% of controls.
- Japanese Cohort 2022: 85 Crohn’s patients took 2g fish oil for 6months. Serum C‑reactive protein (CRP) dropped by an average of 2.1mg/L, and 55% reported fewer bowel movements.
- UK Real‑World Survey 2023: 452 patients on maintenance therapy added 2g EPA/DHA. 42% said they needed fewer corticosteroid bursts over the following year.
While not every study showed dramatic benefits, the trend is consistent: EPA‑rich fish oil can blunt inflammation and support remission, especially when combined with standard medication.
Choosing the Right Form - EPA vs DHA vs Plant‑Based ALA
Not all omega‑3s are created equal for colitis. EPA appears to be the most potent anti‑inflammatory agent, while DHA contributes more to barrier integrity. ALA, on the other hand, must be enzymatically converted - a process that yields only about 5-10% EPA and 2-5% DHA in most adults.
| Attribute | EPA | DHA | ALA (plant‑based) |
|---|---|---|---|
| Primary anti‑inflammatory action | Strong - converts to resolvins | Moderate - converts to protectins | Weak - low conversion rate |
| Barrier support | Moderate | Strong - enhances cell membrane fluidity | Minimal |
| Typical therapeutic dose (combined) | 2-3g EPA | 1-2g DHA | 5-10g ALA (high intake) |
| Best food sources | Mackerel, sardines, salmon | Salmon, tuna, algae oil | Flaxseed, chia seeds, walnuts |
For most patients, a high‑EPA fish oil or a refined EPA/DHA concentrate is the most efficient way to hit the therapeutic window.
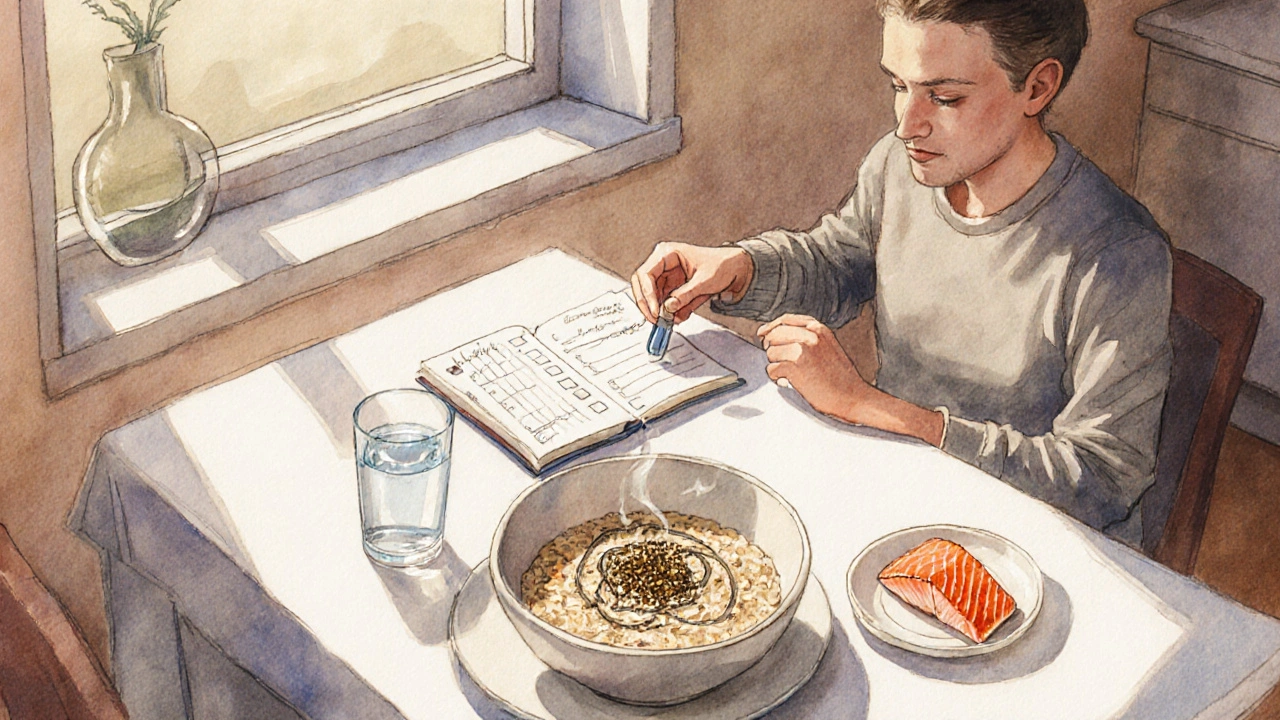
Practical Ways to Add Omega‑3s to Your Routine
- Supplement choice: Look for “EPA‑rich” fish oil capsules with at least 500mg EPA per serving. Verify that the product is third‑party tested for oxidation.
- Dosing schedule: Take the total daily dose split into two meals. Fat‑soluble absorption improves with food.
- Food first: Aim for two servings of fatty fish per week (e.g., 150g grilled salmon). Add a tablespoon of ground flaxseed to oatmeal or smoothies for extra ALA.
- Combine with probiotics: A 2024 trial showed that pairing fish oil (2g EPA/DHA) with a multi‑strain probiotic reduced flare frequency by an additional 15%.
- Monitor labs: Check serum triglycerides and vitaminD levels every 3-6months; omega‑3s can modestly lower triglycerides and improve vitaminD status.
Safety Profile and Possible Interactions
Omega‑3s are generally safe, but be aware of the following:
- Bleeding risk: High doses (>4g EPA/DHA) can inhibit platelet aggregation. If you’re on anticoagulants (e.g., warfarin) or antiplatelet drugs, keep total omega‑3 intake under 2g unless your doctor advises otherwise.
- Gastrointestinal symptoms: Some people experience fishy aftertaste, burping, or mild nausea. Enteric‑coated capsules can help.
- Contaminants: Choose reputable brands that test for mercury and PCBs.
- Pregnancy: EPA/DHA are beneficial for fetal brain development, but stay within recommended limits (≤2g/day) to avoid excess omega‑3.
Putting It All Together - A Sample 4‑Week Plan
- Week1: Start with 1g EPA/DHA (one capsule) taken with dinner. Add a salmon dinner twice this week.
- Week2: Increase to 2g EPA/DHA (two capsules). Incorporate a tablespoon of ground flaxseed into breakfast.
- Week3: Maintain 2g EPA/DHA. Add a probiotic (e.g., Lactobacillusrhamnosus GG) daily.
- Week4: Evaluate symptoms. If flare‑ups have reduced, continue the regimen; otherwise, consult your gastroenterologist about adjusting dose or adding a targeted EPA concentrate.
Tracking a simple diary - noting bowel movements, pain scores, and any side‑effects - can help you and your doctor see whether the plan is working.
Frequently Asked Questions
Can omega‑3s replace my prescription medication?
No. Omega‑3s are an adjunct therapy. They can lower the need for steroids or biologics in some patients, but they don’t cure colitis on their own.
Is fish oil safe for children with ulcerative colitis?
Yes, at lower doses (about 500mg EPA/DHA per day) and under pediatric guidance. Studies show modest reductions in disease activity without major side‑effects.
What if I’m vegetarian? Can I still benefit?
Algae‑derived DHA/EPA supplements provide the same active forms without fish. Combine them with ALA‑rich foods, but remember conversion rates are low, so a direct DHA/EPA source is preferable.
How long does it take to see an improvement?
Most trials report noticeable symptom relief after 8-12weeks of consistent dosing. Patience and adherence are key.
Should I avoid any foods while taking omega‑3 supplements?
Limit excessive saturated fats and processed meats, as they can counteract anti‑inflammatory benefits. A balanced Mediterranean‑style diet works best.
Remember, every body reacts differently. Use the information here as a roadmap, but always keep your gastroenterology team in the loop when you tweak your regimen.

