Quercetin Medication Interaction Checker
Check Your Medication Safety
This tool helps you understand if your medications could interact with quercetin supplements. Enter your medication name below to see risk level and recommendations.
Risk Level:
Metabolized By:
Potential Consequences
Recommendations
Quercetin is everywhere these days. You’ll find it in capsules labeled "natural immune support," in green tea extracts, and even in some fruit-based energy powders. But here’s the part most people don’t know: if you’re taking prescription meds, quercetin could be quietly changing how your body handles them-sometimes dangerously.
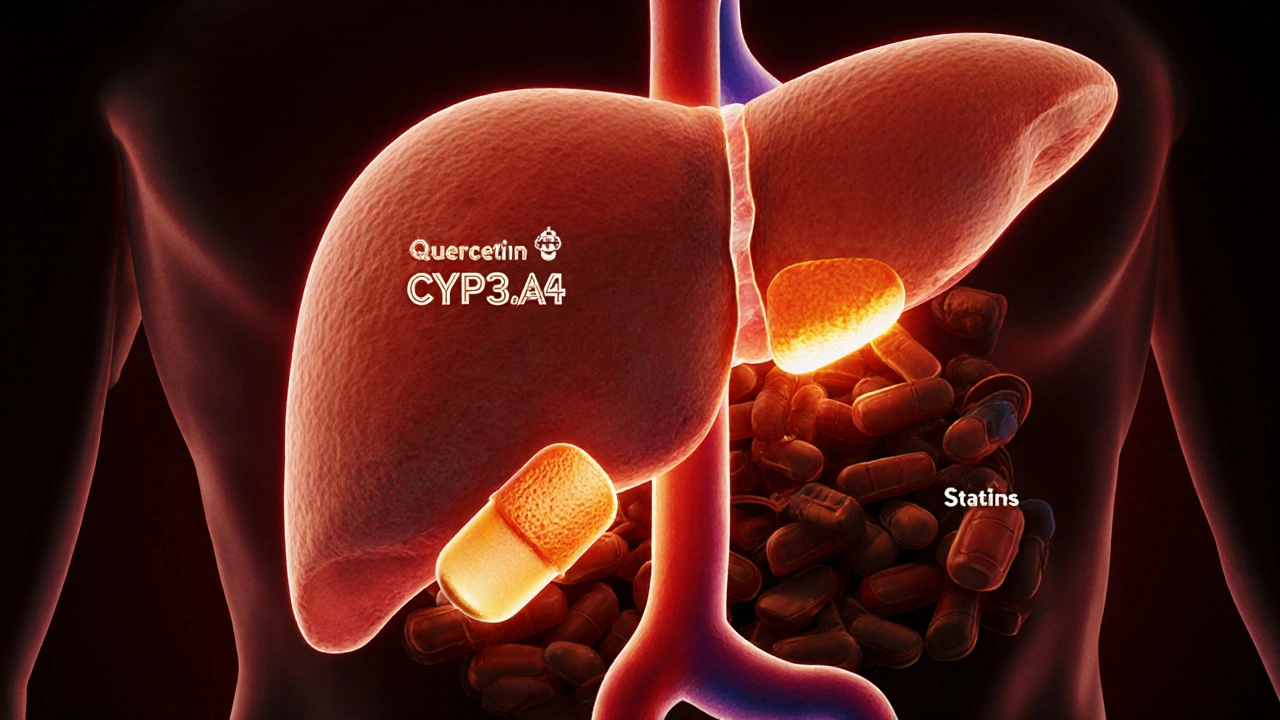
What Quercetin Actually Does to Your Liver
Quercetin isn’t just a plant pigment. It’s a powerful inhibitor of enzymes your liver uses to break down drugs. Specifically, it targets the CYP450 family-CYP3A4, CYP2D6, and CYP2C19. These enzymes are responsible for metabolizing more than half of all prescription medications. When quercetin blocks them, drugs don’t get broken down as quickly. That means they build up in your bloodstream.Think of it like a traffic jam on a highway. Your meds are the cars. The enzymes are the toll booths that let them pass through and exit the system. Quercetin slams those toll booths shut. The result? Higher drug levels than intended.
Studies show quercetin can reduce the metabolism of drugs like abemaciclib (a cancer treatment) by 25-35%, and acenocoumarol (a blood thinner) by 30-45%. In lab tests, it blocked CYP2D6 by up to 85% at concentrations found in people taking high-dose supplements. That’s not theoretical. That’s measurable. And it matters.
Which Medications Are at Risk?
Not all drugs are affected equally. The danger spikes with medications that have a narrow therapeutic index-where the difference between a safe dose and a toxic one is tiny.- Warfarin: Quercetin can raise INR levels by 0.8 to 1.5 points, pushing you into dangerous bleeding territory.
- Cyclosporine: Used after organ transplants, this drug’s levels can jump 30-50% with quercetin, risking kidney damage.
- Abemaciclib, Abrocitinib: These cancer and eczema drugs are metabolized by CYP3A4. Quercetin can raise their blood levels enough to cause severe side effects.
- Direct Oral Anticoagulants (DOACs): Apixaban and rivaroxaban are affected not just by enzyme inhibition but also by transporter interference. The risk of internal bleeding rises sharply.
- Statins: Atorvastatin and simvastatin can accumulate, increasing the chance of muscle damage.
- Antidepressants: SSRIs like sertraline and fluoxetine are processed by CYP2D6. Quercetin can push levels into toxic ranges.
Even common painkillers like acetaminophen aren’t safe. Quercetin can raise their levels by 20-30%. That might sound small, but if you’re already taking the max daily dose, it could push you over the edge into liver injury.
Why Food Isn’t the Problem-Supplements Are
You might be thinking: "I eat apples and onions every day. Why is that okay?"Because the amount of quercetin in food is tiny. A medium onion has about 20-40 mg. An apple? Around 10 mg. Even a cup of kale gives you less than 50 mg. Your body absorbs only a fraction of that-and the rest gets broken down before it ever hits your liver.
But supplements? That’s a different story. A single capsule can contain 500 mg, 1,000 mg, or more. That’s 25 times the amount you’d get from a whole day’s worth of vegetables. And at those doses, quercetin doesn’t just sit there-it actively interferes.
Also, supplements often use pure quercetin aglycone-the most potent form. The kind in food is usually bound to sugar molecules (like rutin), which are far less active. So eating quercetin-rich foods? Fine. Taking quercetin pills? Risky.

Who’s Most at Risk?
It’s not just about the dose. Your body’s ability to clear quercetin matters too.People over 65 clear quercetin metabolites 25-40% slower than younger adults. That means even a 500 mg dose can linger longer, increasing interaction time. If you’re on multiple meds-common in older adults-that’s a recipe for trouble.
Also, people with liver conditions, or those taking drugs that already strain the liver, are more vulnerable. Quercetin doesn’t just interact with drugs-it can add stress to an already overloaded system.
And here’s something no supplement label tells you: quercetin is poorly absorbed. Only 1-2% of what you swallow actually enters your bloodstream. But here’s the catch: even that tiny amount is enough to block enzymes in your gut and liver. You don’t need high blood levels to cause big effects.
What the Experts Say
The European Food Safety Authority (EFSA) warned in 2018 that quercetin supplements over 1,000 mg/day pose "potential concerns" for drug interactions. The FDA listed quercetin as a "dietary supplement of concern" in its 2020 draft guidance, specifically naming CYP3A4, CYP2D6, and CYP2C19 as pathways to monitor.Pharmacists at UCSF developed a clear protocol: avoid quercetin supplements over 500 mg/day if you’re on any medication metabolized by those enzymes. For high-risk drugs like cyclosporine or DOACs, they recommend avoiding it entirely.
And the numbers are growing. In the U.S., nearly 18 million adults took quercetin supplements in 2021. Over 40% of them took more than 500 mg daily. That’s millions of people unknowingly mixing a potent enzyme blocker with their prescriptions.

What You Can Do
If you’re taking quercetin supplements and any prescription meds, here’s what to do:- Stop the supplement. Especially if you’re on blood thinners, cancer drugs, or immunosuppressants.
- Talk to your pharmacist. They have access to drug interaction databases and can check your exact meds. Don’t wait for your doctor to ask-bring it up.
- Don’t assume "natural" means safe. Quercetin is a plant compound, but it acts like a drug. And drugs interact.
- If you must take it, space it out. Taking quercetin 4-6 hours apart from your meds can reduce interaction risk by 30-50%, according to modeling studies. But this isn’t a guarantee.
- Watch for symptoms. Unusual bruising, dizziness, nausea, muscle pain, or confusion could signal a drug buildup. Get tested if you notice them.
The bottom line: quercetin isn’t harmless. At supplement doses, it’s a pharmacological agent with documented, measurable effects on drug metabolism. And the people most likely to take it-those seeking "natural" health boosts-are often the same ones on multiple prescriptions.
What’s Next?
The FDA is working on new labeling rules for supplements like quercetin, expected by 2025. Until then, the burden is on you. Don’t rely on labels that say "supports immunity" or "anti-inflammatory." If it’s a supplement with 500 mg or more of quercetin, and you’re on any medication, assume it’s interacting.There’s no shortcut here. Natural doesn’t mean safe. And when your life depends on a drug working just right, you can’t afford to guess.
Can I still eat foods high in quercetin like onions and apples if I take medications?
Yes. The amount of quercetin in whole foods is too low to cause significant enzyme inhibition. You’d need to eat over 10 pounds of onions daily to reach the dose that interferes with drugs. Stick to normal portions-there’s no need to avoid these healthy foods.
Is quercetin safe if I don’t take any medications?
For healthy people not on any prescription drugs, quercetin supplements are generally considered low-risk at doses under 1,000 mg/day. But long-term safety data is limited. There’s no proven benefit for most people that outweighs the unknown risks. If you don’t need it, don’t take it.
How do I know if my medication is affected by quercetin?
Check if your drug is metabolized by CYP3A4, CYP2D6, or CYP2C19. Common ones include statins, antidepressants, blood thinners, immunosuppressants, and some cancer drugs. Your pharmacist can look this up using a drug interaction database. If you’re unsure, assume it’s risky and ask.
Do all quercetin supplements have the same effect?
No. Supplements vary widely in potency, form, and absorption. Pure quercetin aglycone is the most active form and the most dangerous for interactions. Quercetin bound to sugar (like rutin) is much weaker. But most labels don’t specify the form. If it says "quercetin 500 mg," it’s likely the potent version.
What should I do if I’ve been taking quercetin with my meds?
Stop taking the supplement immediately. Don’t wait for symptoms. Contact your doctor or pharmacist to discuss whether you need a blood test to check your drug levels-especially if you’re on warfarin, cyclosporine, or a DOAC. Most interactions reverse within a few days after stopping quercetin.