When a patient takes theophylline for asthma or COPD, they’re walking a tightrope. Too little, and their breathing doesn’t improve. Too much, and they could have a seizure, a heart attack, or worse. That’s why theophylline levels aren’t just another lab result-they’re a matter of life or death.
What Makes Theophylline So Dangerous?
Theophylline has been used for over 80 years to open up airways in people with asthma and COPD. It works by relaxing smooth muscle in the lungs and reducing inflammation. But unlike most drugs, it doesn’t have a wide safety margin. Its therapeutic window is just 10 to 20 mg/L. That’s a tiny range. At 9 mg/L, the drug might not help at all. At 21 mg/L, serious side effects start to creep in. Above 25 mg/L, the risk of death climbs sharply. This isn’t just theoretical. In the U.S., about 1,500 people end up in emergency rooms every year because of theophylline toxicity. Around 10% of those cases are fatal, usually from irregular heart rhythms or seizures. Even patients who take the same dose as someone else can have wildly different blood levels. One person might need 400 mg daily to stay in range. Another might overdose on 200 mg. Why? Because theophylline doesn’t play by normal rules.Why Monitoring Isn’t Optional
Theophylline’s metabolism is chaotic. It’s broken down in the liver by enzymes that get thrown off by just about everything: smoking, alcohol, other medications, age, liver disease, even pregnancy. - A smoker clears the drug 50-70% faster than a non-smoker. If they quit, their levels can spike dangerously within days. - A 65-year-old with reduced liver function may need half the dose of a healthy 30-year-old. - Taking an antibiotic like ciprofloxacin or erythromycin can boost theophylline levels by 60-100%. - Pregnancy lowers clearance by 30-50% in the third trimester. - Drinking alcohol can drop levels unpredictably. These aren’t rare edge cases. They’re everyday clinical realities. A patient might have been stable for months-until they got a cold, started a new antibiotic, or stopped smoking. Without a blood test, you’d never know.When and How to Monitor
Monitoring isn’t a one-time thing. It’s ongoing. Here’s when to check:- Five days after starting the drug-or three days after any dose change-to let levels stabilize.
- Every 3-6 months for healthy adults on a steady dose.
- Every 1-3 months for patients over 60, with heart failure, or liver disease.
- Monthly during pregnancy, especially in the second and third trimesters.
- Immediately if symptoms appear: nausea, vomiting, tremors, rapid heartbeat, confusion.
- After starting or stopping any new medication, especially antibiotics or antifungals.
What Else to Watch For
Blood levels alone don’t tell the whole story. You need to look at the whole picture:- Heart rate: Over 100 bpm can signal early toxicity.
- Electrolytes: Theophylline often runs with other drugs like albuterol or steroids that drain potassium. Low potassium worsens arrhythmia risk.
- Respiratory rate: Rapid breathing can mean the body is struggling.
- Blood gases: To check for worsening hypoxia or acidosis.
- Full blood count: Rare, but theophylline can suppress bone marrow over time.
Real Cases, Real Consequences
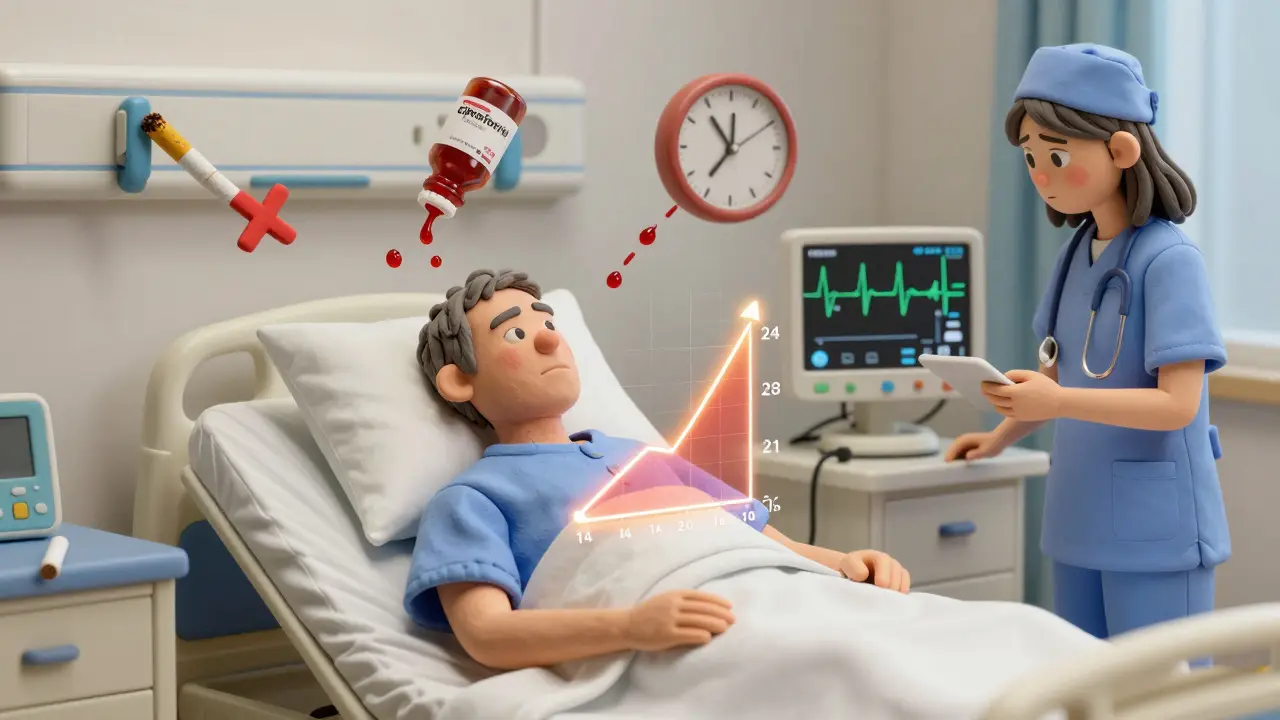
In 2023, a 68-year-old man with COPD was doing fine on 300 mg of theophylline daily. Then he got a urinary tract infection and was prescribed ciprofloxacin. Within three days, his theophylline level jumped from 14 mg/L to 28 mg/L. He developed ventricular tachycardia and had to be hospitalized. His antibiotics weren’t the problem-they were the trigger. Without monitoring, he’d have died. On the flip side, a 2022 study in a community hospital showed that after implementing a strict monitoring protocol, adverse events dropped by 78%. Asthma control improved by 35%. Patients who got regular tests were far more likely to stay out of the ER.

