When you buy a hearing aid, you’re not just buying a device-you’re buying better hearing. But here’s the truth most people don’t know: real-ear measurements aren’t optional. They’re the difference between hearing something and actually understanding it.
What Real-Ear Measurements Actually Do
Real-ear measurements (REM) are the only way to know exactly how much sound your hearing aid is delivering inside your own ear canal. It’s not guesswork. It’s not software simulation. It’s a direct, physical measurement of sound pressure levels-right where your eardrum is.
Every ear is different. The shape, length, and width of your ear canal change how sound travels. One person’s ear might naturally boost high frequencies by 15 dB. Another’s might absorb them. If your hearing aid is programmed based on an average ear-like the 2cc test coupler used in factories-you’re probably getting the wrong amount of amplification. Studies show this leads to mismatches of 8 to 20 dB across key speech frequencies. That’s not a small error. That’s missing half the words in a conversation.
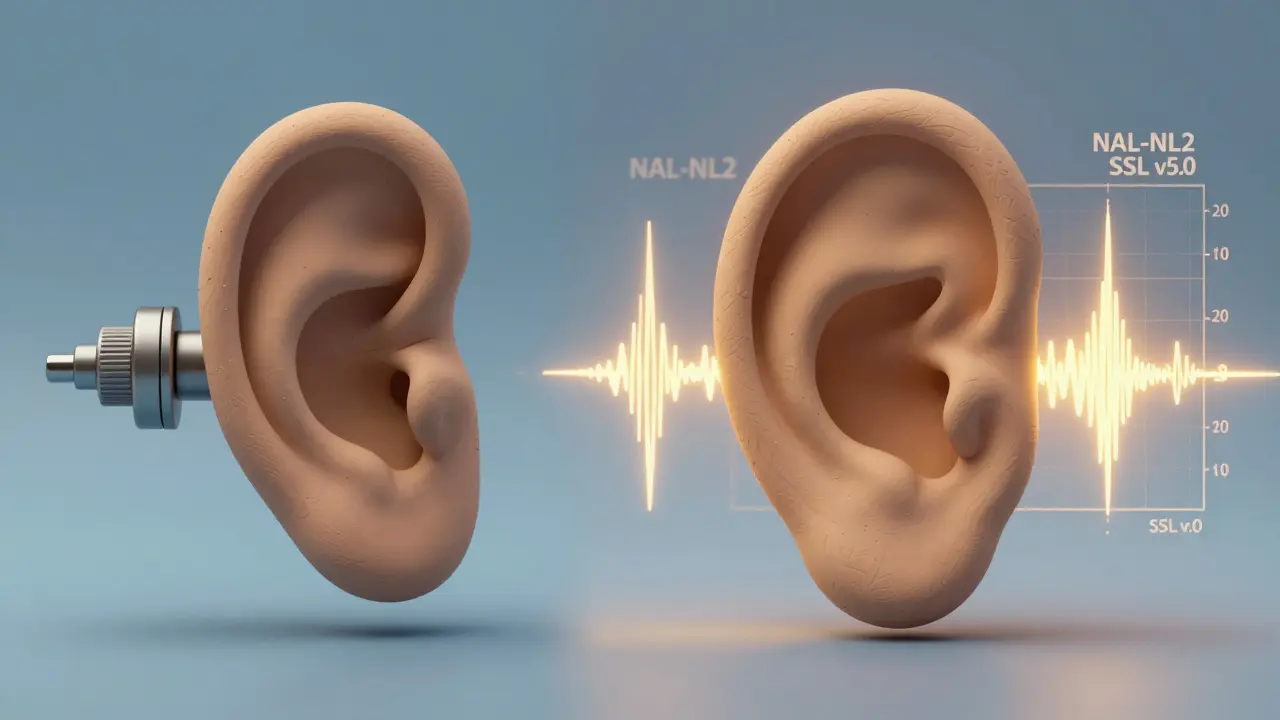
REM fixes that. A thin probe tube, thinner than a strand of hair, is placed just 5 mm from your eardrum. The hearing aid goes in. A speaker plays speech sounds at different volumes-50 dB (quiet), 65 dB (normal), 80 dB (loud). Microphones measure exactly what your ear hears. The software compares that to your personal hearing loss profile and the target amplification rules like NAL-NL2 or DSL v5.0. If the hearing aid isn’t hitting the mark, it’s adjusted-on the spot.
Why Manufacturer ‘First Fit’ Isn’t Enough
Most hearing aids come with a default setting called a ‘first fit.’ It’s based on your audiogram and a generic ear model. It’s quick. It’s easy. And it’s wrong for most people.
According to MarkeTrak data from 2021, only 52% of first-fit settings match the target gain needed for clear speech. That means nearly half the time, you’re getting too little amplification in the frequencies you need most-or too much, causing discomfort or feedback. Even advanced software from brands like Oticon or Phonak only correlates at 65% with real-ear performance. That’s like using a map of London to navigate Tokyo.
Compare that to REM. When done properly, REM achieves 92% accuracy against target gain. That’s not a slight improvement. That’s going from barely hearing your grandchild to understanding every word they say at the dinner table.
The Cost of Skipping Verification
Some people avoid REM because they think it’s expensive or time-consuming. It adds 15 to 25 minutes to your fitting appointment. But here’s what skipping it really costs you.
Patients who get REM are 35% better at understanding speech in noisy places like restaurants or group gatherings. That’s not a minor perk. That’s independence. That’s not having to ask people to repeat themselves constantly. That’s not avoiding social events because listening is exhausting.
And it saves money in the long run. A 2021 study found that patients who had REM done had 43% fewer follow-up visits for adjustments. Why? Because the hearing aid was right the first time. No more returning for ‘a little more volume’ or ‘less buzzing.’
Meanwhile, people who buy over-the-counter (OTC) hearing aids without professional fitting report higher rates of frustration. One Trustpilot review from April 2023 said: ‘Saved $1,000. They whistle constantly. I gave up.’
What Happens During the Test
The process is simple, but precision matters.
- First, your audiologist checks your ear canal with an otoscope. If there’s wax, infection, or a perforation, REM can’t be done safely.
- Then, the probe tube is gently inserted. It’s not painful-just a slight tickling sensation. About 22% of first-timers notice it, but 98% say it’s brief and tolerable.
- The hearing aid is placed in your ear, keeping the probe tube in position.
- Soft sounds, normal speech, and loud speech are played through a calibrated speaker in a sound-treated room.
- The system measures the output at each frequency and compares it to your target curve.
- Adjustments are made. The test is repeated until the output matches your prescription.
It’s not magic. It’s science. And it’s required by the American Speech-Language-Hearing Association (ASHA), the American Academy of Audiology (AAA), and the American Medical Association (AMA). In fact, Medicare and most private insurers cover REM under CPT code 92597 because they recognize it as a medical necessity.
Who Doesn’t Use REM-and Why It Matters
Not all hearing aid providers are created equal. Audiologists-who have doctoral training and are licensed healthcare professionals-use REM in 89% of fittings, according to the 2022 American Academy of Audiology survey. Hearing instrument specialists-who often work in retail chains-use it in only 12% of cases.
Why the gap? Training. REM requires skill. You need to know how to position the probe tube correctly. You need to understand prescriptive targets. You need to interpret complex graphs. That takes 40 to 60 hours of specialized training. Many retail settings don’t invest in that.
And here’s the kicker: hospital-based audiology departments use REM in 98% of cases. Independent practices? 76%. Retail stores? Often below 20%. If you’re getting a hearing aid from a kiosk or a big-box store, chances are you’re not getting REM. And that means you’re not getting the best possible outcome.
What’s Changing in 2026
The field is evolving. In 2023, the European Union made REM mandatory for all hearing aids sold in the region under ISO 12121:2023. The FDA’s 2022 OTC rule explicitly states these devices cannot replace professional evaluation. And in the U.S., the National Institutes of Health are funding $2.4 million in research to make REM faster and more automated.
New tools are emerging. Widex’s MOMENT 2 system uses AI to analyze REM data in real time, cutting fitting time by 30%. 3D ear scanning is getting better-but experts agree: no scan can replace actual sound measurement. As Dr. Pamela Souza said in her 2022 keynote: ‘No matter how advanced our modeling becomes, we’ll always need to verify what’s actually happening in the real ear.’

What Patients Say
On HealthyHearing.com’s 2022 survey of over 1,200 users, 87% of those who had REM said their hearing aids were ‘very effective.’ Only 52% of those without REM said the same.
One Reddit user, ‘HearingHelp42,’ wrote: ‘The REM process was slightly uncomfortable but knowing my aids were precisely calibrated made all the difference-I went from struggling in restaurants to understanding 90% of conversations.’
Another common theme? Reduced listening effort. Nearly 70% of users reported feeling less tired after conversations. That’s not just about hearing louder. It’s about hearing clearly-and that takes energy. When your brain doesn’t have to work so hard to fill in the gaps, you have more mental bandwidth for everything else.
What to Ask Before Your Fitting
If you’re getting a hearing aid, don’t leave without asking these questions:
- Will you be using real-ear measurements to verify the fit?
- Which prescriptive target will you use-NAL-NL2 or DSL v5.0?
- Will you show me the before-and-after graphs?
- Do you have a sound booth that meets ANSI standards?
- Will you test at 50, 65, and 80 dB speech levels?
If the answer to any of these is ‘no,’ walk away. You’re paying for a medical device. You deserve medical-grade verification.
Final Thought
Hearing aids aren’t like glasses. You can’t just pick a strength and call it done. Your ears are complex, dynamic systems. What works for one person won’t work for another. Real-ear measurements are the only way to close the gap between theory and reality. They’re not a luxury. They’re the standard. And if your provider won’t use them, you’re not getting the best care. You’re getting a guess.
Are real-ear measurements painful?
No, real-ear measurements are not painful. A thin probe tube is placed near the eardrum, which may cause a mild tickling sensation for some people-about 22% of first-time patients report this. But it’s brief, lasting only a few minutes during the test. Over 98% of patients say the discomfort is tolerable and worth the result.
Can I skip REM if I’m buying OTC hearing aids?
The FDA explicitly warns that over-the-counter (OTC) hearing aids are not a substitute for professional evaluation and fitting. Without REM, you have no way to know if the device is delivering the right amount of amplification for your unique hearing loss and ear anatomy. Many OTC users report feedback, discomfort, or poor speech understanding because the device wasn’t verified for their ears. REM is the only reliable method to ensure proper performance.
Why do some providers say REM isn’t necessary?
Some providers, especially in retail settings, skip REM to save time or reduce costs. But this isn’t about convenience-it’s about standards. The American Speech-Language-Hearing Association, the American Academy of Audiology, and the American Medical Association all state that REM is the gold standard. If a provider claims it’s optional, they’re not following professional guidelines. Ask why they don’t use it. If they can’t give you a credible answer, look elsewhere.
Is REM covered by insurance?
Yes, REM is covered by Medicare and most private insurers under CPT code 92597. The American Medical Association classifies it as a medical necessity because it directly affects the success of hearing aid treatment. If your provider says it’s not covered, ask them to verify the billing code. You have a right to this verification.
How long does a real-ear measurement take?
The REM process typically takes 15 to 25 minutes during a hearing aid fitting. This is added to the initial consultation and programming time. While it extends the appointment, it reduces the need for multiple follow-up visits. Patients who get REM have 43% fewer adjustments needed later, saving time and frustration in the long run.
Can I get REM if I have earwax or an ear infection?
No. Before REM can be performed, your audiologist must check your ear canal with an otoscope. If there’s significant earwax, infection, or a perforated eardrum, the test cannot be done safely. These issues must be treated first. This is why a proper pre-fitting exam is essential-it’s not just a formality, it’s a safety step.
Do children need real-ear measurements too?
Yes. In fact, REM is even more critical for children. Their ear canals are smaller and change rapidly as they grow. The 2023 Joint Committee on Infant Hearing states that REM is essential for all pediatric fittings. Without it, children may not receive the precise amplification needed for speech and language development. Delayed or inaccurate fitting can impact learning and communication for years.
What’s the difference between REM and coupler testing?
Coupler testing measures hearing aid output in a fake ear-a 2cc plastic box designed to represent an ‘average’ ear canal. It’s used in manufacturing and quality control. REM measures sound pressure in your actual ear canal, accounting for your unique anatomy. Coupler tests can be off by 8-20 dB. REM is accurate to within ±2 dB. One is a factory check. The other is a personalized medical verification.
Can I see the results of my REM test?
Absolutely. A good audiologist will show you the graphs before and after adjustment. You’ll see your hearing loss curve, the target amplification line, and the actual output from your hearing aid. If the two lines match closely, you know your device is working as intended. If not, they’ll adjust it until they do. This transparency is part of professional care.
Is REM worth the extra time and cost?
Yes. The extra 20 minutes and any small additional cost are an investment in your quality of life. Patients who get REM report significantly better speech understanding, less listening fatigue, and higher satisfaction. They’re also less likely to return the device or give up on hearing aids altogether. In the long run, REM saves money, time, and frustration-and gives you the hearing you deserve.