Getting life-saving medication shouldn’t mean choosing between rent and refills. For millions of Americans, patient assistance programs from drug companies are the only way to afford prescriptions. But qualifying isn’t simple. Even if you’re struggling, you might be denied because you didn’t know the exact rules - or because you have insurance you didn’t realize disqualifies you.
Who Can Actually Get Help?
The biggest myth about these programs is that they’re for anyone who can’t afford medicine. That’s not true. Most programs only help people who are uninsured or underinsured - meaning they have Medicare, Medicaid, or commercial insurance that doesn’t cover their specific drug, or they pay too much out of pocket even with coverage. If you’re completely uninsured, you’re in luck. Many manufacturer programs like Pfizer’s Patient Assistance Program and Merck’s program specifically target this group. But here’s the catch: if you have private insurance - even if it’s terrible - you’re often automatically disqualified. Some programs, like AbbVie’s, won’t even let you apply if your insurer says you must use their PAP first. Medicare beneficiaries face a whole different set of rules. If you’re on Medicare Part D and your income is below 150% of the Federal Poverty Level (about $20,385 for one person in 2023), you’re supposed to get Extra Help from Medicare. But if you’re denied Extra Help - or you’re in that gray zone between 135% and 150% FPL - you might fall through the cracks. Programs like Takeda’s Help At Hand require you to submit proof that Medicare turned you down before they’ll even look at your application.Income Limits Are the Key - But They’re Not Simple
Income is the most common filter. Nearly every program uses a percentage of the Federal Poverty Level (FPL). For 2023, 500% FPL meant $75,000 for a single person and $153,000 for a family of four. But here’s where it gets messy:- Pfizer’s RxPathways uses 300% FPL ($43,200) for basic meds like Eucrisa, but 500-600% FPL ($64,800-$77,760) for cancer drugs.
- GSK sets a hard cap at $58,650 for one person and $120,570 for four people.
- Merck allows hardship exceptions for insured patients who earn under 400% FPL - but only if they can prove extreme financial distress.
Insurance Status Can Block You - Even If You’re Broke
This is the hardest part to understand. Independent charities like the PAN Foundation and HealthWell Foundation have stricter income limits but more flexible insurance rules. Manufacturer programs? Not so much. A 2019 study found 97% of independent charity PAPs exclude the uninsured - the very people who need help most. Meanwhile, Pfizer, GSK, and others require you to be uninsured or on government programs like Medicaid. If you have a commercial plan - even if it has a $10,000 deductible - you’re often out of luck. There’s one exception: new “commercial PAPs” launched by 12 major drugmakers since 2022. These are designed for people with insurance who still pay too much out of pocket. If your copay is $500 a month for a diabetes drug, you might qualify. But these are new, limited, and not available for every medication.
What Documents Do You Need?
You can’t just say you’re poor. You have to prove it. Every program requires:- A completed application signed by you and your doctor
- Proof of income: W-2s, pay stubs, tax returns, or Social Security award letters
- Proof of U.S. residency: utility bill, lease, or driver’s license
- Proof of U.S. treatment: prescription from a U.S.-licensed doctor
Medicare Part D Creates a Hidden Trap
If you’re on Medicare, you need to understand how PAPs interact with your Part D plan. The government requires PAPs to stay “outside the Part D benefit.” That means the value of free drugs from a manufacturer doesn’t count toward your True Out-of-Pocket (TrOOP) costs. Why does that matter? Because once you hit $8,000 in TrOOP (in 2024), you get catastrophic coverage - your costs drop to almost nothing. But if you’re getting free drugs from Pfizer or GSK, you’re not moving closer to that cap. You’re stuck paying full price until you hit the limit. That’s why some people with Medicare and high drug costs are better off paying out of pocket than using a PAP - at least until they reach the TrOOP threshold. It’s counterintuitive, but it’s real.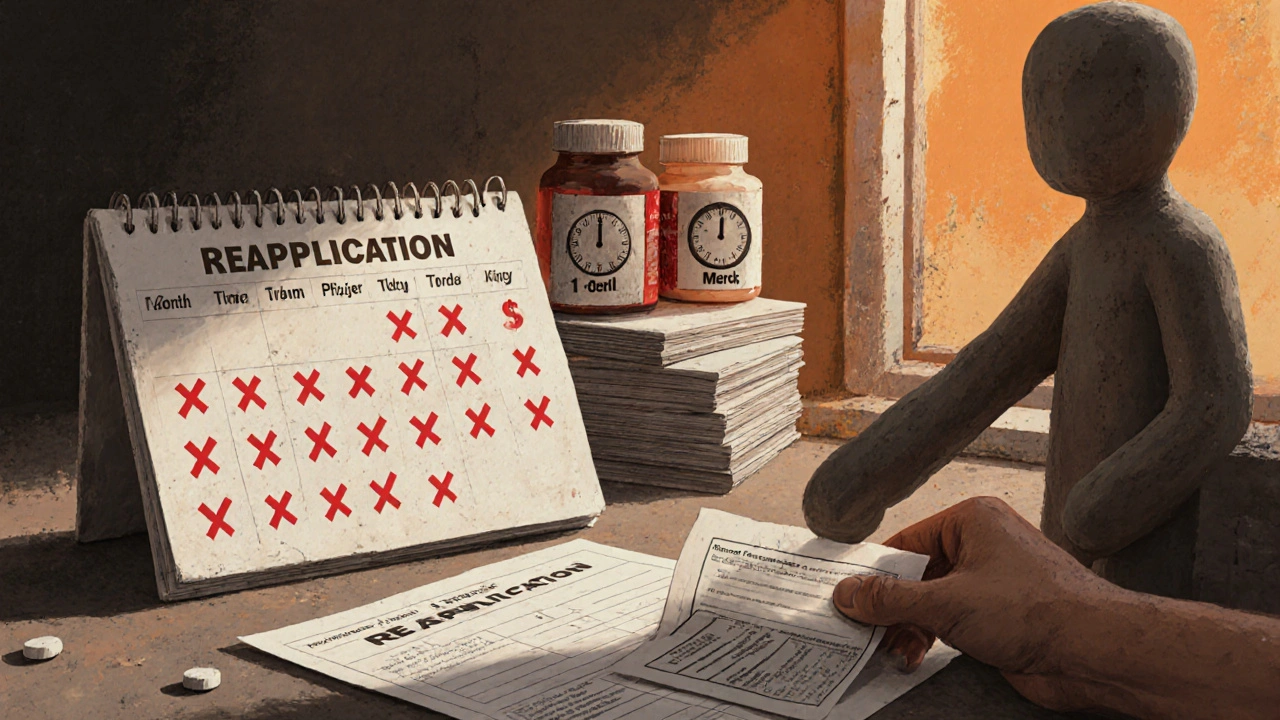
What Happens After You Apply?
Approval isn’t instant. The average processing time is 14.7 days. But denials are common - 37% of first-time applicants get rejected, according to Reddit users and Medicare Rights Center surveys. Most denials happen because of paperwork mistakes: missing signatures, wrong income numbers, or incomplete forms. If you’re denied, don’t give up. Nearly half of successful applicants had to reapply three or more times. The most common fix? Submitting updated tax documents or getting a clearer letter from your doctor. Once approved, you’ll usually get your meds within 72 hours. But you’ll need to reapply. For most drugs, you re-enroll every year. For specialty or cancer meds, you might need to re-verify every three months. GSK requires annual reapplication. Pfizer asks for income updates every six months.What If You Don’t Qualify?
If you’re turned down, you still have options:- Check with independent charities like PAN Foundation or HealthWell Foundation - they sometimes help people with insurance.
- Ask your pharmacist about patient support programs - many pharmacies partner with PAP navigators.
- Use the Medicine Assistance Tool (MAT) from NeedyMeds.org - it scans dozens of programs at once.
- Call your drugmaker’s customer service line. Sometimes they have unlisted hardship programs.
Bottom Line: Know the Rules Before You Apply
Patient assistance programs aren’t free money. They’re complex, inconsistent, and full of traps. But for those who qualify, they’re the difference between life and death. Don’t assume you’re ineligible because you have insurance. Don’t assume your income is too high. Don’t skip the doctor’s signature. And don’t give up after one denial. The system is broken - but it still works for those who know how to play it.Can I get free medicine if I have Medicare?
Yes - but only if you meet strict income limits and your drug isn’t covered by your Part D plan. Some programs require you to first apply for Medicare’s Extra Help and get denied before you qualify. Others won’t help you at all if you’re on Medicare Part D. Always check the specific program’s rules.
Do I need to be completely uninsured to qualify?
Most manufacturer programs do require you to be uninsured or on government programs like Medicaid. But some newer programs, launched since 2022, now help people with commercial insurance who face high out-of-pocket costs. Check the specific drugmaker’s site - eligibility varies by medication.
What if my income is just above the limit?
Some programs allow hardship exceptions if you can prove medical or financial distress - like high medical bills, eviction, or job loss. Merck and a few others consider these cases. You’ll need detailed documentation, including bills, letters from landlords, or unemployment records.
How long does approval take?
On average, it takes 14-21 days. Some programs approve in as little as 72 hours if you submit everything correctly. Delays usually come from waiting for your doctor to sign forms or for income documents to be verified. Use online portals like Pfizer’s RxPathways to speed things up.
Do I have to reapply every year?
Yes. Most programs require annual re-enrollment. For specialty or cancer drugs, you may need to re-verify every 3-6 months. GSK and Pfizer both require updated income proof yearly. Missing a deadline means your medication stops - no warning.
Can I apply for multiple programs at once?
Yes. You can apply to several manufacturer programs and independent charities simultaneously - as long as you meet each one’s rules. Many people use one program for a cancer drug and another for a diabetes medication. Just make sure you don’t double-dip on the same drug from multiple sources.