Insulin Regimen Selector
Which Insulin Regimen Fits Your Life?
This tool analyzes your daily routine to determine whether basal-bolus or premixed insulin might better suit your needs based on scientific research and real-world experience.
Your Recommendation
Key Considerations:
Choosing between basal-bolus and premixed insulin isn’t just about numbers on a glucose meter. It’s about whether you can stick with it when your schedule gets messy, when you’re tired, or when your blood sugar drops in the middle of the night. The right insulin plan doesn’t just control your blood sugar-it fits your life. And the side effects? They’re not the same for everyone.
How Basal-Bolus Insulin Works
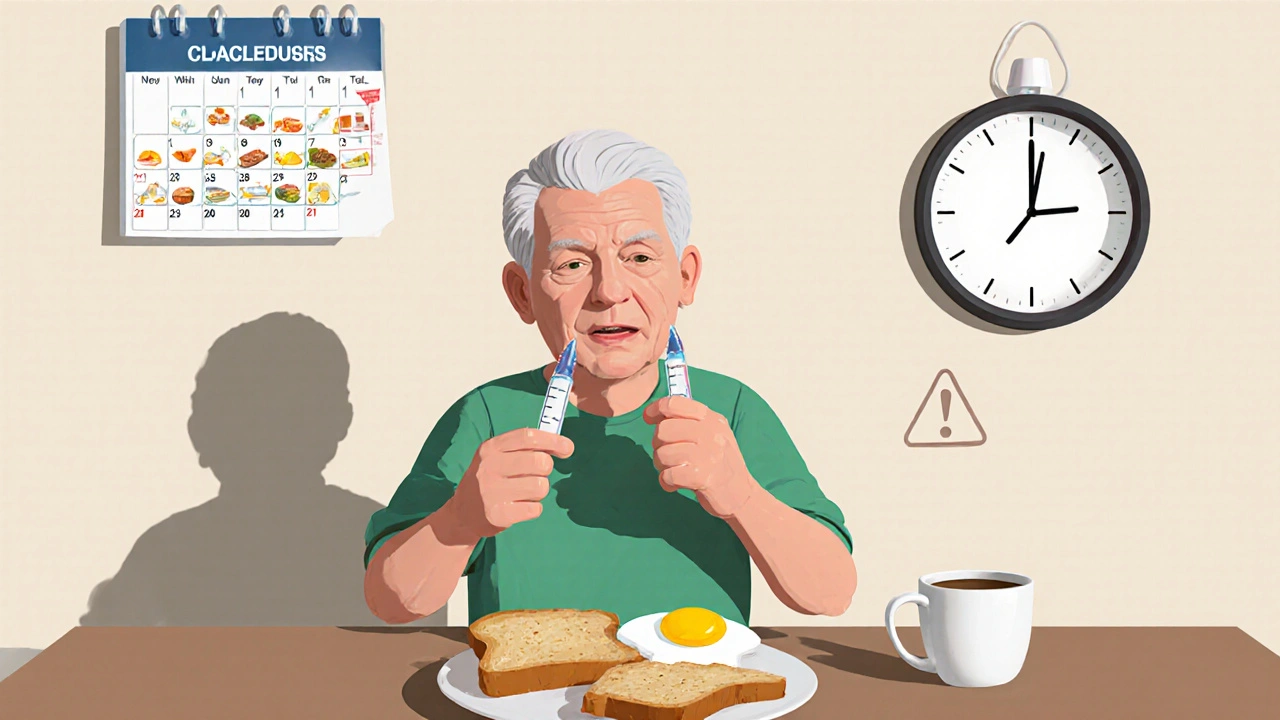
Basal-bolus therapy means two kinds of insulin working together. One is long-acting, called basal insulin, which keeps your blood sugar steady between meals and overnight. The other is rapid-acting, called bolus insulin, taken right before meals to handle the sugar spike from food. Most people need four to five injections a day: one or two for basal, and one before each meal plus an extra correction dose if needed.This system gives you control. Eat a big pasta dinner? Take more bolus. Skip lunch? Skip the bolus. Got a late-night snack? You can cover it. That flexibility is why it’s the gold standard for type 1 diabetes and many with type 2 who need tight control. But it’s not simple. You need to count carbs, check your blood sugar before every meal, and adjust doses based on what you eat and how active you are. It’s a lot of math, and it takes time to get good at it.
How Premixed Insulin Works
Premixed insulin is a one-two punch in a single shot. It combines a fixed amount of intermediate-acting insulin (like NPH) with rapid- or short-acting insulin. Common ratios are 70/30 or 75/25-meaning 70% long-acting, 30% fast-acting. You typically take it twice a day, before breakfast and dinner. Some people take it three times a day if they eat more frequently.It’s simpler. No carb counting. No guessing how much to take before each meal. Just two or three shots, same time, same dose. That’s why it’s popular with older adults, people with memory issues, or those who find multiple daily injections overwhelming. But here’s the catch: you have to eat the same amount of carbs at the same time every day. Miss a meal? Your blood sugar can crash. Eat more than usual? You’re stuck with high blood sugar until your next shot.
Side Effects: Hypoglycemia Is the Big Difference
The biggest worry with any insulin is low blood sugar. And here’s where basal-bolus and premixed diverge sharply.Studies show premixed insulin carries a higher risk of hypoglycemia-especially at night and between meals. Why? Because the long-acting part doesn’t last evenly. NPH peaks around 4-8 hours after injection, which can cause a sudden drop if you haven’t eaten or if you’re active. A 2015 trial had to stop early because over half the people on premixed insulin had dangerous lows. That’s not a small risk-it’s a safety alarm.
Basal-bolus users have lower rates of nighttime lows. Why? Their basal insulin (like glargine or degludec) releases slowly and steadily, without big peaks. They only take fast-acting insulin when they eat. So if they skip a meal, they skip the bolus. No insulin, no crash. That’s a big deal for people who work night shifts, have unpredictable schedules, or just don’t always feel hungry.
Weight Gain: It’s Not as Big a Deal as You Think
People often worry insulin makes them gain weight. That’s true-but not equally true for both regimens.Studies show basal-bolus users gain slightly more weight on average-about 1.9 kg over time-compared to 1.0 kg with premixed. Why? Because basal-bolus lets you eat more freely. You can cover higher-carb meals without fear of spikes, so you might eat more. Premixed users, on the other hand, are stuck with fixed portions. They can’t easily adjust, so they often eat less to avoid highs.
But here’s the real story: weight gain isn’t about the insulin itself. It’s about how much you eat and how active you are. If you’re eating more because you feel better (no more glucose spikes and crashes), that’s not necessarily bad. It’s your body finally getting the fuel it needs.
Lifestyle Fit: Flexibility vs Routine
This is where the real battle lies-not in the lab, but in your kitchen, your car, your job, your social life.Basal-bolus wins for flexibility. Need to eat dinner at 9 p.m. after work? No problem. Going out for pizza on Friday? Take your bolus. Traveling across time zones? Adjust your basal dose. You’re not chained to a clock. But this freedom comes at a cost: you need to be willing to learn, track, and think about food constantly. It’s not for everyone.
Premixed insulin demands routine. You eat breakfast at 8 a.m., lunch at 1 p.m., dinner at 6 p.m. You can’t skip. You can’t delay. You can’t change your mind. That’s fine if you’re retired, live alone, and eat the same meals every day. But if you’re a parent, a shift worker, or someone who eats on the go? You’ll feel trapped. One Reddit user wrote: “I switched from premixed to basal-bolus because missing a meal meant risking hypoglycemia-even if my sugar was normal.” That’s not a small frustration. It’s a daily stressor.
On the flip side, many older adults say premixed saved their lives. One 78-year-old on the ADA forum said: “Two shots a day instead of four has made managing my diabetes possible since my arthritis makes multiple injections painful.” For them, simplicity isn’t a compromise-it’s survival.
Cost and Accessibility Matter
Let’s talk money. Basal-bolus usually costs more. You’re buying two or three separate insulin products: basal, rapid-acting, and sometimes a backup pen. Medicare data shows average monthly out-of-pocket costs of $68.20 for basal-bolus versus $45.75 for premixed.That gap matters. In the U.S., it’s a barrier. In parts of Asia, where premixed insulin is used in over half of cases, cost and access drive the choice. In the UK and Europe, basal-bolus adoption is rising fast-not because it’s cheaper, but because technology is making it easier.
Technology Is Changing the Game
You don’t have to do all the math yourself anymore.Continuous glucose monitors (CGMs) have changed everything. A 2022 study found that CGM users on premixed insulin had hypoglycemia rates nearly cut in half-down to just 0.2 events per month. That’s because they see their glucose dropping before it becomes dangerous. They can eat a snack, pause, or adjust.
And now there’s AI. Systems like Diabeloop’s DBLG1 can analyze your glucose trends and suggest insulin doses automatically. Early trials show patients using AI tools need 27% fewer decisions per day. That’s huge. It’s turning basal-bolus from a complex chore into a smart assistant.
Even new insulins are helping. The FDA approved a “basal-plus” option in 2023-a single injection that gives you steady basal coverage with the option to add a quick bolus if you eat more. It’s a middle ground for people who want flexibility without five daily shots.
Who Gets Which Regimen?
There’s no one-size-fits-all. But guidelines give clear clues.Basal-bolus is best for:
- People with type 1 diabetes
- Those with high post-meal spikes
- People who eat irregular meals or travel often
- Those willing to learn carb counting and use a CGM
- Anyone who wants the tightest possible control
Premixed insulin is best for:
- Older adults with arthritis or memory issues
- People with very consistent daily routines
- Those with limited access to diabetes education
- Patients who fear multiple injections
- Those in areas where insulin costs are high and CGMs aren’t available
The American Diabetes Association says it plainly: choose based on your life, not just your numbers. Your doctor should ask: “Can you stick with this?” not just “Will it lower your HbA1c?”
What If You’re Not Sure?
Start with what’s easiest to manage. If you’re new to insulin, premixed might be a good first step. But don’t stay there if it’s making you anxious, hungry, or scared of lows.Many people start on premixed, then switch to basal-bolus when they realize they’re missing meals, gaining weight, or feeling restricted. Others start with basal-bolus and go back to premixed because the daily workload is too much.
There’s no shame in switching. Insulin therapy isn’t a life sentence-it’s a tool. And tools should fit your hands, not force you to reshape your life for them.
Ask your doctor for a trial. Try one regimen for 8-12 weeks. Track your lows, your energy, your meals, your stress. See what works. Then adjust. You’re not failing if you change plans. You’re being smart.

