PPI Recommendation Tool for DAPT Patients
Personalized PPI Recommendation Tool
Based on the latest guidelines (2023 ESC), determine if you need a PPI and which one is safest for your antiplatelet therapy.
Which antiplatelet therapy are you on?
Do you have risk factors for GI bleeding?
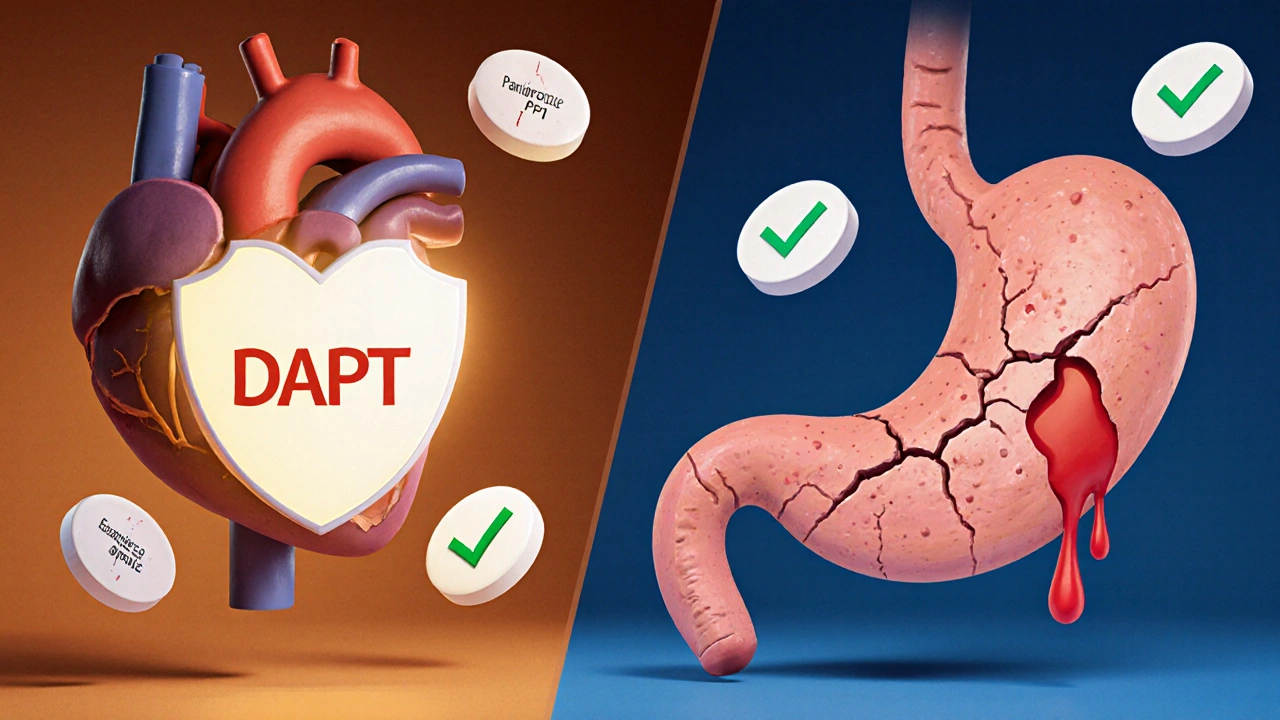
When you're on dual antiplatelet therapy-usually aspirin plus clopidogrel, prasugrel, or ticagrelor-your blood doesn't clot as easily. That’s good for preventing heart attacks and strokes. But it also means your stomach is more vulnerable. Up to 50% of people on this combo will develop a gastrointestinal bleed within the first year. That’s not just discomfort. It’s hospitalization. Sometimes death.
The solution isn’t to stop the blood thinners. It’s to protect the stomach. That’s where proton pump inhibitors (PPIs) come in. Used correctly, PPIs slash the risk of serious GI bleeding by a third to nearly 40%. But here’s the catch: not all PPIs are created equal. And using the wrong one can undo the benefits of your heart medication.
Why DAPT Increases GI Bleeding Risk
Dual antiplatelet therapy (DAPT) is standard after a heart stent, heart attack, or certain strokes. Aspirin blocks platelets from sticking together. Clopidogrel, prasugrel, or ticagrelor block a different pathway. Together, they’re powerful. But that same power irritates the stomach lining and reduces protective mucus. The result? Ulcers. Bleeding. Emergency endoscopies.
Studies show the risk jumps 30-50% in the first 30 days. Most bleeds happen early. A 2025 Korean study of nearly 97,000 patients found that 75% of major GI bleeds occurred within the first month of starting DAPT. That’s why timing matters. You don’t wait for symptoms. You start protection right away.
How PPIs Work-And Why They’re So Effective
PPIs like omeprazole, esomeprazole, and pantoprazole shut down the acid pumps in your stomach. These pumps, called H+/K+ ATPase, are what make stomach acid. When you take a PPI, acid production drops by 70-98%. Less acid means less damage to irritated tissue. Less chance of an ulcer turning into a bleed.
It’s not magic. It’s science. The COGENT trial, published in JAMA in 2010, followed over 3,000 patients on DAPT. Half got a PPI. The other half didn’t. The group with the PPI had 34% fewer GI bleeds. That’s one major bleed prevented for every 71 patients treated. In real terms? That’s dozens of lives saved every day in the U.S. alone.
And it’s not just aspirin. PPIs work whether you’re on 81 mg or 325 mg of aspirin. They work with clopidogrel. They work with ticagrelor. They work with prasugrel. The protection is consistent.
The Big Problem: Omeprazole and Clopidogrel
Here’s where things get tricky. Omeprazole-the cheapest and most commonly prescribed PPI-interferes with clopidogrel. Both are processed by the same liver enzyme: CYP2C19. When omeprazole blocks this enzyme, clopidogrel can’t turn into its active form. That means your blood thinners don’t work as well.
Studies show omeprazole reduces clopidogrel’s effect by up to 45%. A 2010 meta-analysis in Circulation found this translated to a 27% higher risk of heart attack or stroke in patients taking both. That’s not worth the trade-off.
So if you’re on clopidogrel, avoid omeprazole. Don’t take it. Don’t ask for it. Don’t accept it if your doctor suggests it without knowing the risk.
The Right PPIs for the Right DAPT
Not all PPIs mess with clopidogrel. Pantoprazole and esomeprazole barely touch CYP2C19. In fact, they reduce clopidogrel’s effectiveness by less than 15%-so little it’s considered clinically irrelevant.
Here’s the simple rule:
- If you’re on clopidogrel → Use pantoprazole 40 mg daily or esomeprazole 20-40 mg daily.
- If you’re on prasugrel or ticagrelor → You can safely use any PPI, including omeprazole. These drugs don’t rely on CYP2C19, so there’s no interaction.
That’s it. No guesswork. No trade-offs. Just matching the right drug to the right therapy.

PPIs vs. H2 Blockers: Why PPIs Win
You might wonder: why not use famotidine or ranitidine? They’re cheaper. They’re available over the counter. They reduce acid too.
But they’re not as good. A 2017 meta-analysis in JAMA Internal Medicine compared PPIs to H2 blockers in patients on DAPT. PPIs cut GI bleeding risk by 60%. H2 blockers? Only 30%. That’s a 50% difference in protection. In absolute terms, PPIs prevented 1.8% more bleeds than H2 blockers. That’s not small. That’s life or death.
Plus, H2 blockers lose effectiveness over time. Your body gets used to them. PPIs don’t. They stay strong all day, every day.
Who Really Needs a PPI?
Not everyone on DAPT needs a PPI. But many think they do. And many doctors overprescribe them.
The 2023 European Society of Cardiology guidelines say: give a PPI if you have two or more of these risk factors:
- History of GI bleed or ulcer
- Age 65 or older
- Taking anticoagulants (like warfarin or apixaban)
- Taking NSAIDs (ibuprofen, naproxen)
- Taking corticosteroids
If you’re 50, healthy, no prior ulcers, not on other meds-chances are you don’t need it. But if you’re 72, had a bleed five years ago, and take aspirin plus ibuprofen for arthritis? You absolutely do.
Here’s the scary part: a 2022 study found 35-45% of DAPT patients on PPIs had no risk factors. They were taking it for no reason. And that’s dangerous.
The Hidden Risks of Taking PPIs Too Long
PPIs are safe for months. Maybe a year. But years? That’s where problems start.
Long-term use (over 1 year) has been linked to:
- Cl. diff infection - Risk goes up by 0.5%. That’s small, but serious. Cl. diff causes severe diarrhea, hospitalization, even death.
- Community-acquired pneumonia - Risk increases by 0.8%. Acid normally kills bacteria in the stomach. Less acid means more bacteria can travel up.
- Chronic kidney disease - Risk rises 20%. The exact reason isn’t clear, but the link is real.
- Bone fractures - Especially in older women. Long-term acid suppression affects calcium absorption.
The FDA has issued warnings about these risks. That’s why guidelines say: use the lowest dose for the shortest time. Most patients only need it for 6-12 months. After that, reassess.

What About the Newer Drugs?
There’s a new kid on the block: vonoprazan. It’s not a PPI. It’s a potassium-competitive acid blocker (P-CAB). It works faster. It’s stronger. And it doesn’t interact with clopidogrel at all.
In a 2024 trial called VENOUS, vonoprazan was just as good as esomeprazole at preventing GI bleeds-but with zero CYP2C19 interference. The FDA is reviewing it for approval in late 2025. If approved, it could become the new gold standard.
Until then, stick with pantoprazole or esomeprazole. They’re proven. They’re cheap. They work.
How to Make Sure You’re Getting the Right Treatment
You’re not just a patient. You’re your own best advocate. Here’s what to do:
- Ask your doctor: "Which PPI are you prescribing, and why?"
- Confirm which antiplatelet you’re on: clopidogrel, prasugrel, or ticagrelor?
- If it’s clopidogrel, insist on pantoprazole or esomeprazole. Say no to omeprazole.
- Ask: "How long should I take this?" Don’t let it become a lifelong habit unless you have ongoing risk.
- Get your risk score checked. If you have two or more risk factors, PPI is justified. If not, question it.
Many doctors don’t know the interaction details. A 2022 survey found 45% of cardiologists were unsure which PPIs were safe with clopidogrel. Don’t assume they do. Bring the facts.
Cost, Access, and Real-World Gaps
Pantoprazole costs less than $5 a month as a generic. Esomeprazole is $10-15. Omeprazole is $3. But if you take omeprazole with clopidogrel, you’re risking a heart attack. That’s not savings. That’s costlier care down the road.
Even with low cost, underuse is a problem. In Korea, only 16.6% of low-risk DAPT patients got a PPI-even though guidelines say they should. In the U.S., only 42% of hospital systems use real-time risk tools to guide prescribing.
This isn’t about money. It’s about precision. We know who needs it. We know what to give them. We just aren’t doing it consistently.
Bottom Line: Do This Now
If you’re on DAPT:
- Don’t skip the PPI if you’re at risk. Your stomach matters as much as your heart.
- Don’t take omeprazole if you’re on clopidogrel. It’s dangerous.
- Choose pantoprazole or esomeprazole. They’re safe and effective.
- Ask how long you need it. Most people don’t need it forever.
- Don’t take it if you have no risk factors. You’re exposing yourself to side effects for no benefit.
This isn’t a one-size-fits-all situation. It’s a precision medicine moment. The right PPI, at the right time, for the right person, saves lives. The wrong one? It can cost them.
Can I take omeprazole with clopidogrel?
No. Omeprazole blocks the liver enzyme (CYP2C19) that clopidogrel needs to become active. This can reduce clopidogrel’s effectiveness by up to 45%, increasing your risk of heart attack or stroke. Use pantoprazole or esomeprazole instead.
Do I need a PPI if I’m on ticagrelor or prasugrel?
You still need a PPI if you have risk factors for GI bleeding (age 65+, prior ulcer, on NSAIDs or anticoagulants). But you can safely use any PPI-including omeprazole-because ticagrelor and prasugrel don’t rely on CYP2C19 for activation.
How long should I take a PPI with DAPT?
Most patients only need it for 6 to 12 months-the period of highest bleeding risk. After that, your doctor should reassess. If you still have risk factors (like ongoing NSAID use), you may need to continue. But don’t stay on it indefinitely without review.
Are H2 blockers like famotidine a good alternative to PPIs?
No. H2 blockers reduce stomach acid, but they’re only about half as effective as PPIs at preventing GI bleeds in patients on DAPT. Studies show PPIs cut bleeding risk by 60%, while H2 blockers only reduce it by 30%. PPIs are the standard for a reason.
Can PPIs cause kidney damage or dementia?
Long-term use (over a year) has been linked to a higher risk of chronic kidney disease and possibly dementia, but the evidence isn’t definitive. The risk is small-about 20% higher for kidney disease and 17% for dementia-but it’s real. That’s why guidelines stress using the lowest dose for the shortest time possible. Don’t take it longer than needed.