Warfarin & NSAID Bleeding Risk Calculator
Input Your Details
Risk Assessment Results
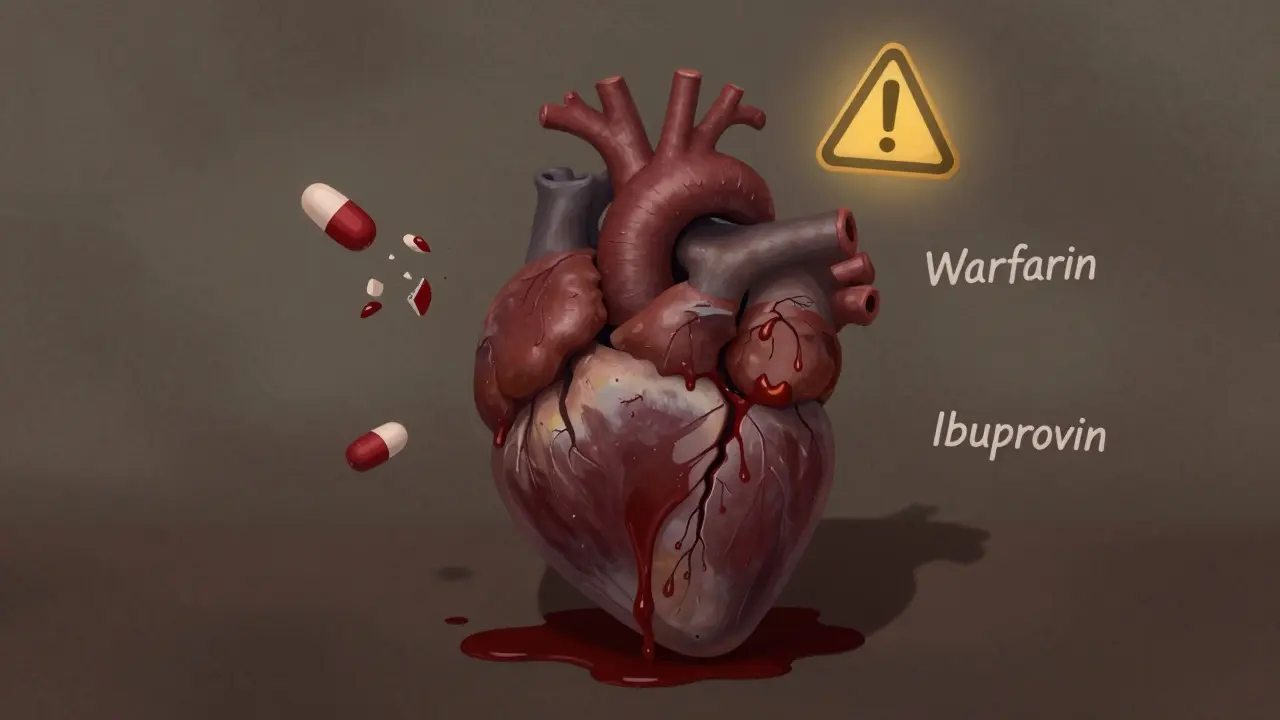
Combining Warfarin and NSAIDs isn’t just a bad idea-it’s dangerous. Thousands of people take both every day, thinking it’s harmless. But the truth is, this mix can send you to the ER with internal bleeding, sometimes with no warning. If you’re on Warfarin for atrial fibrillation, a blood clot, or a mechanical heart valve, and you reach for ibuprofen or naproxen for a headache or sore knee, you’re playing Russian roulette with your blood.
Why This Combination Is So Risky
Warfarin works by blocking vitamin K, which your liver needs to make clotting factors. Without those factors, your blood takes longer to clot-good for preventing strokes, bad if you cut yourself or develop an ulcer. NSAIDs like ibuprofen, naproxen, and diclofenac do two things that make things worse. First, they stop platelets from sticking together properly by blocking COX-1 enzymes. Second, they wear down the stomach lining, making it easier for blood vessels to bleed out.
It’s not just one problem-it’s two broken systems working together. Your blood can’t clot well because of Warfarin, and your platelets can’t form a plug because of the NSAID. At the same time, your stomach is getting eroded. The result? A perfect storm for bleeding.
A 2023 study from Aarhus University Hospital found that people on Warfarin who took NSAIDs had more than double the risk of bleeding compared to those who didn’t. That’s not a small increase. That’s a major jump in danger. And it’s not just stomach bleeding. Brain bleeds, lung bleeds, and urinary tract bleeds all go up too.
Not All NSAIDs Are Created Equal
If you think all NSAIDs are the same, you’re wrong. Some are far more dangerous with Warfarin than others.
- Naproxen increases bleeding risk by 4.1 times compared to Warfarin alone.
- Diclofenac raises it by 3.3 times.
- Ibuprofen is a bit less risky-but still 1.79 times higher.
- Meloxicam is especially risky for people on high-dose Warfarin.
Even if you think you’re being careful by taking a low dose, it doesn’t matter. The risk builds up over time. A single dose can push your INR up enough to cause trouble. One study of 98 Warfarin users found that nearly 40% saw their INR spike by 15% or more after adding an NSAID. That’s enough to turn a minor bruise into a life-threatening bleed.
And no, COX-2 inhibitors like celecoxib aren’t safer. Despite early hopes that they’d spare the stomach and platelets, research shows they carry the same bleeding risk as traditional NSAIDs when mixed with Warfarin. The stomach lining still breaks down. The clotting system still gets hit. The risk doesn’t disappear.
Who’s Most at Risk?
Some people are walking into this trap without even knowing it. Here’s who’s most vulnerable:
- People over 75-risk of bleeding jumps 3.7 times.
- Those on high-dose Warfarin (more than 40 mg per week).
- Anyone taking other meds that affect clotting, like aspirin or SSRIs.
- People with a history of ulcers or GI bleeding.
- Those with low baseline INR-they’re more likely to see a sharp spike when NSAIDs are added.
And here’s the scary part: many of these people don’t even tell their doctor they’re taking NSAIDs. A University of Michigan study found that in 68% of Warfarin-related bleeding cases, patients didn’t mention their OTC painkiller use. They think Tylenol is the only safe option. They don’t realize Advil, Aleve, or even topical NSAID gels can cause trouble.
What About Newer Blood Thinners?
You might have heard that newer anticoagulants like apixaban, dabigatran, or rivaroxaban are safer. And yes, they don’t interact with as many drugs as Warfarin. But that doesn’t mean NSAIDs are okay with them.
A 2019 Circulation study showed NSAIDs still raise bleeding risk with NOACs. The ARISTOTLE trial found that even with apixaban, NSAID use increased major bleeding. A 2020 meta-analysis confirmed that dabigatran and NSAIDs together still carry a higher bleeding risk than dabigatran alone. Rivaroxaban? Same story.
The myth that NOACs = NSAID-safe is spreading fast. In fact, between 2015 and 2022, NSAID use with NOACs went up by 35%. That’s not progress-it’s a new wave of preventable harm. Doctors and patients alike are assuming the newer drugs are bulletproof. They’re not.

Real Stories, Real Consequences
Behind the statistics are people who woke up in the hospital with hemoglobin levels that had dropped from 14 to 8 in under 24 hours. One Reddit user wrote: “Took ibuprofen for a headache. Two days later, I was pale, dizzy, and barely standing. ER said I lost almost half my blood volume.”
Another patient, a 72-year-old with atrial fibrillation, took naproxen for arthritis pain for three days. He didn’t feel any different-until he started coughing up blood. He ended up in the ICU with a pulmonary hemorrhage.
The FDA’s adverse event database recorded over 1,800 bleeding cases linked to Warfarin-NSAID combinations between 2015 and 2020. Sixty-two percent were gastrointestinal. Most required hospitalization. The average stay? Over five days. The cost? $1.87 billion a year in the U.S. alone.
On Drugs.com, the combination has a safety rating of 2.1 out of 10. Eighty-seven percent of reviews warn against it. The advice? “Use Tylenol. Or don’t take anything at all.”
What Should You Do Instead?
You don’t have to suffer in pain. There are safer options:
- Acetaminophen (Tylenol) is the go-to. It doesn’t affect platelets or the stomach lining. Use it at the right dose-no more than 3,000 mg a day if you’re on Warfarin, and avoid alcohol.
- Topical NSAIDs like diclofenac gel may be safer, but they’re not risk-free. Some still get absorbed into the bloodstream. Use with caution.
- Physical therapy, heat packs, or massage can help with chronic joint pain.
- Low-dose capsaicin cream for arthritis pain has no known interaction with anticoagulants.
If you absolutely must take an oral NSAID-say, after surgery or for severe inflammation-talk to your anticoagulation provider first. They’ll likely want to:
- Check your INR before you start.
- Use the lowest possible dose for the shortest time (no more than 3-5 days).
- Avoid naproxen, diclofenac, and meloxicam.
- Start a proton pump inhibitor like omeprazole to protect your stomach.
- Check your INR again in 3-5 days, then weekly while you’re on the NSAID.
And never, ever start an NSAID without telling your doctor or pharmacist you’re on Warfarin-or any other blood thinner.
Why Doctors Still Prescribe This Mix
It’s not because they don’t know the risk. It’s because they’re overwhelmed. Patients come in with bad knees, migraines, or back pain. They’ve been taking ibuprofen for years. The doctor doesn’t have time to dig into their full med list. And EHR systems? Forty-two percent of U.S. hospitals don’t even flag Warfarin-NSAID combinations.
Plus, many patients don’t think of OTC drugs as “medications.” They don’t mention Advil. They don’t think of it as part of their regimen. That’s why so many bleeding events happen quietly-no one connects the dots until it’s too late.

What’s Changing?
Good news: co-prescribing of Warfarin and NSAIDs dropped 27% between 2015 and 2022. That’s because more people are switching to NOACs. But the bad news? NSAID use with NOACs went up. People think they’re safe now. They’re not.
The 2024 American College of Chest Physicians guidelines will be even stricter: no NSAIDs with any oral anticoagulant. Period. Especially for those over 75. The Institute for Safe Medication Practices says there’s no safe way to combine them. If you need pain relief, find another way.
Final Takeaway
Warfarin and NSAIDs don’t mix. Not even a little. The risk isn’t theoretical. It’s proven, measured, and deadly. Your pain matters. But your life matters more.
If you’re on Warfarin or any blood thinner, skip the ibuprofen. Skip the naproxen. Skip the diclofenac. Use acetaminophen. Talk to your pharmacist before taking anything new. Ask your doctor if your pain can be managed without pills at all.
This isn’t about being perfect. It’s about being smart. One pill can change everything. Don’t gamble with your blood.
Can I take Tylenol instead of NSAIDs while on Warfarin?
Yes, acetaminophen (Tylenol) is generally safe to use with Warfarin because it doesn’t affect platelets or the stomach lining like NSAIDs do. However, avoid high doses-stick to no more than 3,000 mg per day-and never mix it with alcohol, as this can increase liver stress and raise your INR. Always check with your doctor if you’re taking it regularly.
Do topical NSAIDs like diclofenac gel carry the same risk?
Topical NSAIDs are absorbed into the bloodstream in smaller amounts, so they’re less risky than oral versions. But they’re not risk-free. Studies show that even topical diclofenac can raise INR in some people, especially with long-term use or large application areas. If you use them, monitor your INR closely and avoid using them daily for weeks at a time.
Is it safe to take NSAIDs occasionally if my INR is stable?
No. Even if your INR is stable, adding an NSAID can cause a sudden spike within days. The risk isn’t about how stable you are-it’s about how the drug affects your body’s clotting system. One study showed nearly 40% of patients had a dangerous INR rise after just one NSAID dose. Stability doesn’t protect you.
Why do some doctors still prescribe NSAIDs with Warfarin?
Some doctors may not be fully aware of the latest guidelines, or they’re under pressure to quickly treat pain. Others assume the patient won’t take the NSAID anyway. But the data shows this combination leads to hospitalizations and deaths. Major organizations like the American Heart Association and American College of Cardiology strongly advise against it. If your doctor prescribes it, ask for the evidence-and consider getting a second opinion.
What should I do if I accidentally took an NSAID while on Warfarin?
Stop taking the NSAID immediately. Contact your anticoagulation clinic or doctor and ask to have your INR checked within 3-5 days. Watch for signs of bleeding: unusual bruising, dark or tarry stools, blood in urine, severe headaches, dizziness, or vomiting blood. If any of these happen, go to the ER right away.
Are there any natural alternatives to NSAIDs for pain?
Yes. Turmeric (curcumin) has anti-inflammatory effects and doesn’t interfere with clotting. Ginger tea can help with mild pain and inflammation. Physical approaches like heat therapy, stretching, and physical therapy are also effective for chronic joint or muscle pain. Always check with your provider before starting any supplement, even natural ones.
How often should I get my INR checked if I’m on Warfarin and need an NSAID?
If NSAID use is unavoidable, check your INR before starting, then again 3-5 days after starting, and weekly while taking it. After stopping the NSAID, check once more in 3-7 days to make sure your INR returns to baseline. Never assume your INR is stable just because you feel fine.
What to Do Next
If you’re on Warfarin, take five minutes today and review your medicine cabinet. Look for any NSAIDs-ibuprofen, naproxen, aspirin, diclofenac. Even if you haven’t used them in months, they’re still a risk if you start again. Talk to your pharmacist or doctor about safer pain options. Ask if your current pain meds are listed in your anticoagulation care plan.
Don’t wait for a bleed to happen. This interaction is predictable, preventable, and deadly. You don’t need to suffer. You just need to be informed.