Adverse Drug Reaction: What It Is, How It Happens, and What to Do
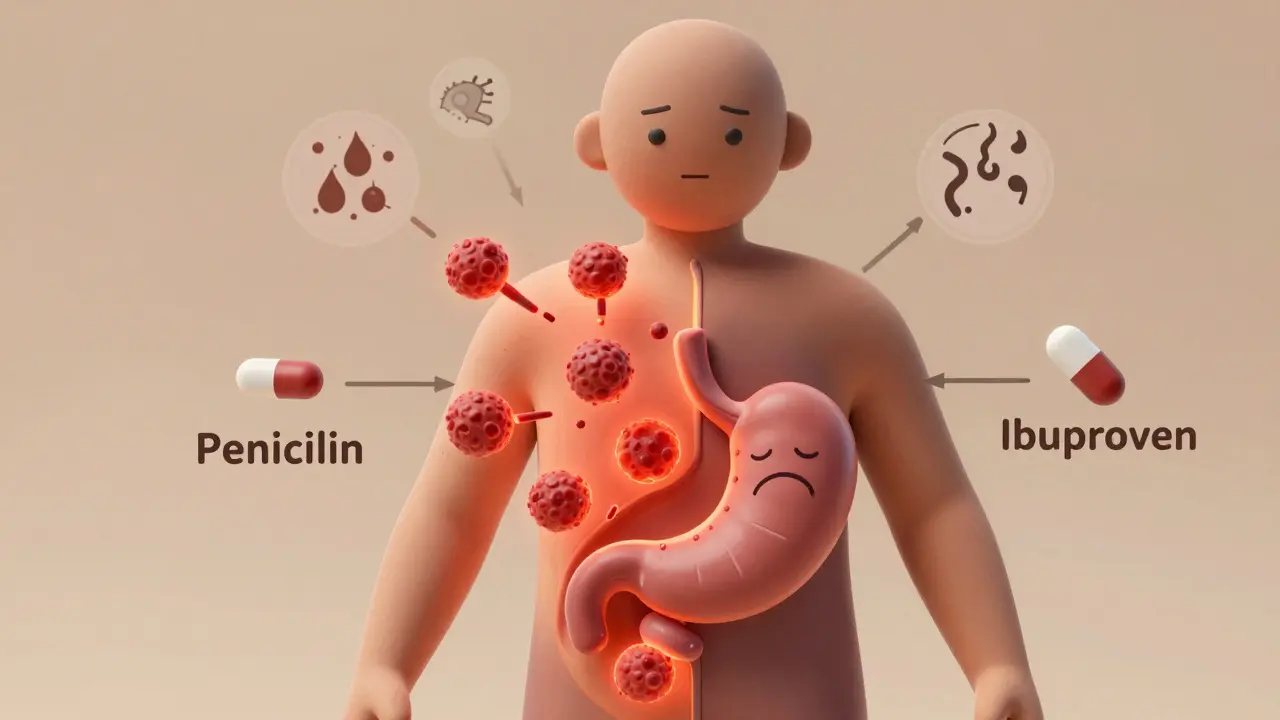
When you take a medication, you expect it to help—not hurt. But sometimes, even the right drug at the right dose can cause unexpected harm. This is called an adverse drug reaction, an unintended and harmful response to a medicine taken at normal doses. Also known as drug side effect, it’s not always an allergy—it can be a chemical mismatch, a genetic quirk, or a dangerous interaction with another pill you’re taking. These reactions don’t always show up right away. Some hit within minutes, like a rash or swelling. Others creep in over days or weeks—fatigue, dizziness, liver stress, or strange bleeding. They’re not rare. In fact, they’re one of the top causes of hospital visits in adults over 65.
What makes an adverse drug reaction worse? polypharmacy, taking multiple medications at once. If you’re on five or more drugs, your chances of a bad reaction jump sharply. pharmacogenetics, how your genes affect how your body processes drugs, plays a big role too. For example, some people can’t break down warfarin properly because of their CYP2C9 gene, making them prone to dangerous bleeding. Others react badly to antibiotics like cefaclor not because they’re allergic, but because their immune system triggers a Serum Sickness-Like Reaction, a delayed immune response that mimics an allergic reaction but isn’t. These aren’t flukes—they’re predictable if you know what to look for.
Doctors don’t always catch these reactions because they’re often mistaken for new illnesses. A sudden drop in blood pressure? Maybe it’s heart trouble. Unexplained nausea? Must be a stomach bug. But if it started after a new pill, it’s probably the drug. That’s why tracking what you take—and when symptoms begin—is critical. You don’t need to be a scientist to spot a pattern. Keep a simple log: drug name, dose, date started, and any new symptoms. Share it with your pharmacist. They’re trained to catch interactions you might miss.
Some reactions are mild and go away when you stop the drug. Others need emergency care—like amitriptyline overdose, which can shut down your heart. That’s why knowing the warning signs matters. If you feel your throat closing, your skin turning red and blistering, or your heart racing out of nowhere, don’t wait. Get help. And if you’ve had one bad reaction before, make sure every doctor and pharmacist knows. It’s not just about avoiding that one drug—it’s about avoiding similar ones in the same class. A reaction to one antibiotic might mean you’re at risk for others.
What you’ll find in the posts below are real stories, real science, and real fixes. From how genetic testing can prevent dangerous reactions to how caregivers can spot early signs of trouble, these articles give you the tools to stay safe. You’ll learn which drugs are most likely to cause problems, how to tell the difference between a side effect and something worse, and what to do when your medicine stops helping and starts hurting. This isn’t theoretical. It’s what keeps people out of the ER.