It’s easy to think that if a drug makes you feel bad, it’s an allergy. You get nauseous after taking aspirin? Must be allergic. Break out in a rash after amoxicillin? Allergy for sure. But here’s the truth: drug allergy is not the same as a side effect-and mixing them up can put your health at risk.
What’s Really Happening in Your Body?
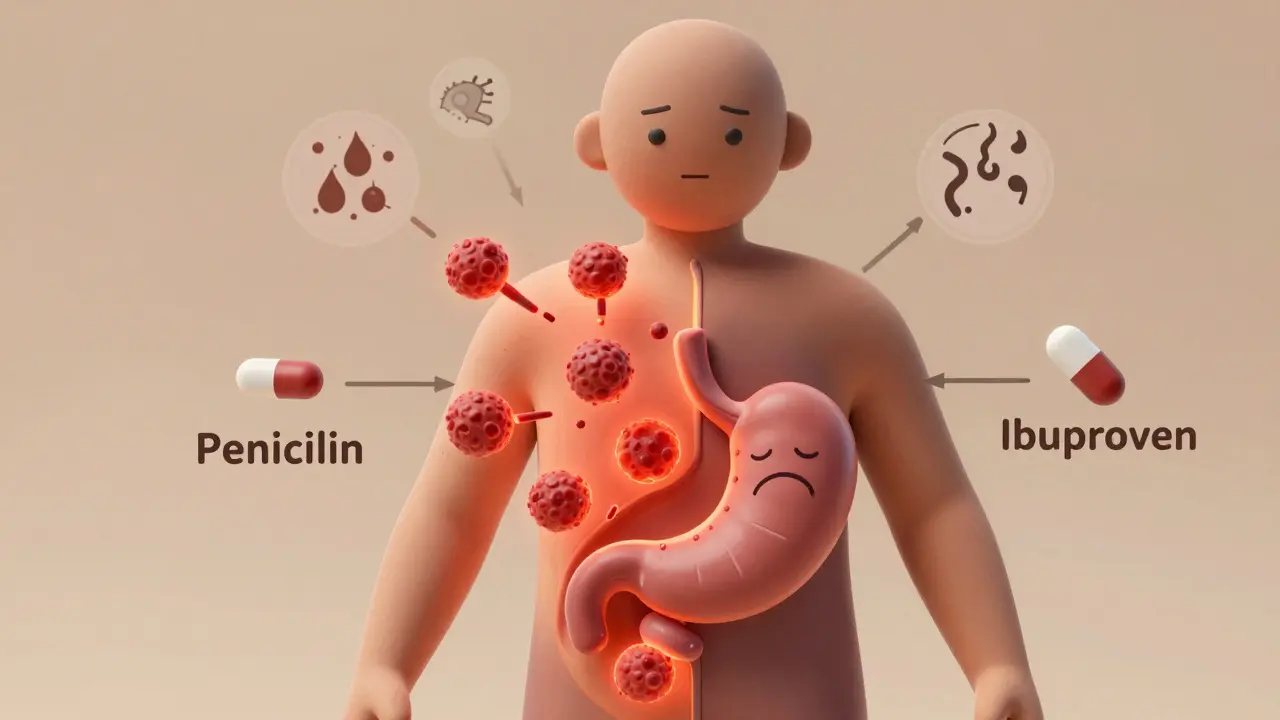
A drug allergy means your immune system thinks the medication is an invader. It responds like it’s fighting off a virus-releasing chemicals like histamine that cause swelling, hives, trouble breathing, or worse. This isn’t just feeling unwell. It’s your body’s defense system going into overdrive.
A side effect, on the other hand, is a direct result of how the drug works. If a pill lowers your blood pressure, it might also make you dizzy. If it kills bacteria in your throat, it might also upset your stomach. These aren’t immune reactions. They’re side notes in the drug’s instruction manual.
The numbers don’t lie. Only 5 to 10% of people who say they have a drug allergy actually have one. That means 9 out of 10 times, someone’s labeling a side effect as an allergy. And that mistake has real consequences.
Timing Tells the Story
When did the reaction happen? That’s your first clue.
If you broke out in hives or felt your throat close up within 30 minutes of taking a pill, that’s a red flag for a true allergy. Immediate reactions are usually IgE-mediated-the classic immune response. These can escalate fast. Anaphylaxis, the most dangerous form, can happen in minutes.
But if you started feeling sick hours or even days later? That’s different. Nausea 2 hours after taking ibuprofen? Classic side effect. A rash that shows up 10 days after starting an antibiotic? That could still be an allergy-but it’s a delayed one, driven by T-cells, not IgE. These are harder to spot, but just as serious.
Side effects tend to show up early, get worse with higher doses, and often fade if you keep taking the drug or lower the amount. Allergies? They get worse with every exposure. The second time you take it, the reaction might be worse than the first.
Symptoms: One System or Many?
Side effects usually stick to one area. Nausea. Headache. Drowsiness. Dry mouth. These are single-system reactions. They’re predictable. Everyone who takes that drug might feel them, at least a little.
True allergies? They rarely stay in one place. If you have a skin rash and swelling in your lips and trouble breathing, that’s a red flag. Multi-system involvement is a hallmark of immune reactions. The same goes for vomiting plus hives, or diarrhea plus wheezing.
According to data from Premier Health, 87% of confirmed drug allergies involved at least two body systems. Only 22% of side effects did. If your reaction crosses lines-skin, lungs, gut-it’s not just a side effect. It’s a signal your immune system is involved.
Penicillin: The Most Misunderstood Allergy
More than 10% of Americans say they’re allergic to penicillin. But here’s the shocker: 90 to 95% of them aren’t.
Most of these people had nausea or a mild rash as kids. They were told, “You’re allergic,” and never questioned it. Years later, they avoid penicillin and get stronger, broader antibiotics instead-drugs that cost more, cause more side effects, and fuel antibiotic resistance.
Studies show people with a mislabeled penicillin allergy have a 69% higher chance of getting a deadly C. diff infection. They also stay in the hospital 30% longer. All because a simple side effect got labeled as an allergy.
That’s why testing matters. Skin tests and drug challenges can confirm or rule out a true penicillin allergy with 95% accuracy. Yet fewer than 1 in 5 people who think they’re allergic ever get tested. That’s not just outdated-it’s dangerous.
When to Worry: The Dangerous Ones
Not all allergic reactions are hives and itching. Some are life-threatening-and they’re easy to miss if you don’t know what to look for.
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are rare but deadly immune reactions. They start with flu-like symptoms, then the skin begins to blister and peel-like a severe burn. These reactions usually happen 1 to 3 weeks after starting a drug. Common culprits: sulfa antibiotics, seizure meds, and NSAIDs.
DRESS syndrome is another delayed reaction: fever, swollen lymph nodes, liver damage, and a widespread rash. It can show up 2 to 6 weeks after taking a drug. Both SJS and DRESS require emergency care and permanent avoidance of the trigger.
If you’ve ever had a drug reaction that made you feel like you were dying-chest tightness, throat closing, passing out-that’s anaphylaxis. It’s not a side effect. It’s an emergency. You need an epinephrine auto-injector and a plan for next time.

What You Can Do Right Now
You don’t need to be a doctor to start sorting this out. Here’s what to do:
- Write down exactly what happened: What drug? When? What symptoms? How long did they last?
- Ask yourself: Was it just one symptom? Or did your skin, breathing, and stomach all go wrong at once?
- Did it get worse the next time you took it?
- Did it happen within an hour? Or days later?
If you’re unsure, talk to your doctor or an allergist. Don’t just assume. Don’t avoid meds out of fear. Get tested.
Many hospitals now have pharmacist-led allergy clinics. They review your history, run simple tests, and help you remove false labels from your chart. At Mayo Clinic, 92% of low-risk patients who were retested could safely take penicillin again.
Why This Matters Beyond You
This isn’t just about your next prescription. It’s about the whole system.
When doctors avoid penicillin because of a false allergy, they reach for stronger, more expensive drugs. That drives up healthcare costs by $500 to $1,000 per patient every time. Across the U.S., it adds up to $1.1 billion a year.
It also makes antibiotic resistance worse. Broader-spectrum drugs kill more good bacteria, letting superbugs grow. That’s not just your problem. It’s everyone’s.
That’s why the FDA now requires drug labels to clearly separate side effects from allergies. And why electronic health records must store this info accurately by January 2025.
Correct labeling saves lives. It saves money. It protects public health.
Final Thought: Don’t Guess. Find Out.
Feeling sick after a pill doesn’t mean you’re allergic. It might just mean the drug isn’t perfect for your body. But if your immune system is involved? That’s different. That’s serious.
Don’t let a childhood rash or a bad stomach upset define your medical future. Ask for a review. Ask for a test. Ask for clarity.
You deserve the right treatment-not the one you’re stuck with because someone labeled a side effect as an allergy.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Up to 80% of people who had a true penicillin allergy as children lose it over time, even without testing. But you shouldn’t assume it’s gone. The only way to know for sure is through a supervised challenge test. Never restart a drug you were once allergic to without medical supervision.
If I’m allergic to one antibiotic, am I allergic to all of them?
No. Allergies are specific to the drug or its chemical structure. Being allergic to penicillin doesn’t mean you’re allergic to amoxicillin, ciprofloxacin, or azithromycin. They’re different molecules. Cross-reactivity does happen sometimes-especially within the same drug class-but it’s not automatic. An allergist can test for specific sensitivities.
Can a side effect turn into an allergy?
No. A side effect is a pharmacological reaction-it’s not immune-based. But you can develop a true allergy to a drug even if you’ve taken it safely before. Your immune system can change over time. That’s why someone might take amoxicillin for years without issue, then suddenly develop hives on the 5th dose. It’s not the side effect turning into an allergy-it’s a new immune response forming.
What if I had a rash but no other symptoms?
A rash alone doesn’t confirm an allergy. Many rashes from drugs are non-allergic, especially if they’re mild and appear after several days. But if the rash is itchy, spreading, or accompanied by fever or blistering, it could be a sign of a serious immune reaction like DRESS or SJS. Don’t ignore it. See a doctor. Even if it seems minor, it’s worth getting checked-especially if you need that drug again.
Can I take the drug again if I only had nausea?
Yes, likely. Nausea is one of the most common side effects-not an allergy. If you’ve only had stomach upset, dizziness, or fatigue, you probably can take the drug again. But talk to your doctor first. They might suggest lowering the dose, taking it with food, or switching to a different formulation. Avoiding a drug unnecessarily limits your treatment options and can lead to worse outcomes.