When you’re diagnosed with sleep apnea, your doctor might recommend a breathing device. Two of the most common options are CPAP and BiPAP. They both use air pressure to keep your airway open while you sleep, but they’re not the same. Choosing the wrong one can make therapy uncomfortable-or even ineffective. So what’s the real difference? And more importantly, which one is right for sleep apnea treatment in your case?
How CPAP Works
CPAP stands for Continuous Positive Airway Pressure. It delivers one steady stream of air pressure from the moment you turn it on until you turn it off. That pressure is set just high enough to stop your airway from collapsing during sleep. For most people with obstructive sleep apnea, this single pressure works perfectly.
Typical CPAP pressure ranges from 4 to 20 cm H₂O. The machine doesn’t adjust during the night-it just keeps pushing air at the same level. That’s simple. And for about 85% of people with obstructive sleep apnea, it’s all they need.
Modern CPAP devices like the ResMed AirSense 11 or Philips DreamStation 2 are quiet, lightweight, and come with built-in humidifiers. Many include smart features like automatic pressure adjustment, leak detection, and therapy tracking. But the core function hasn’t changed since the 1980s: constant pressure to keep your throat open.
How BiPAP Works
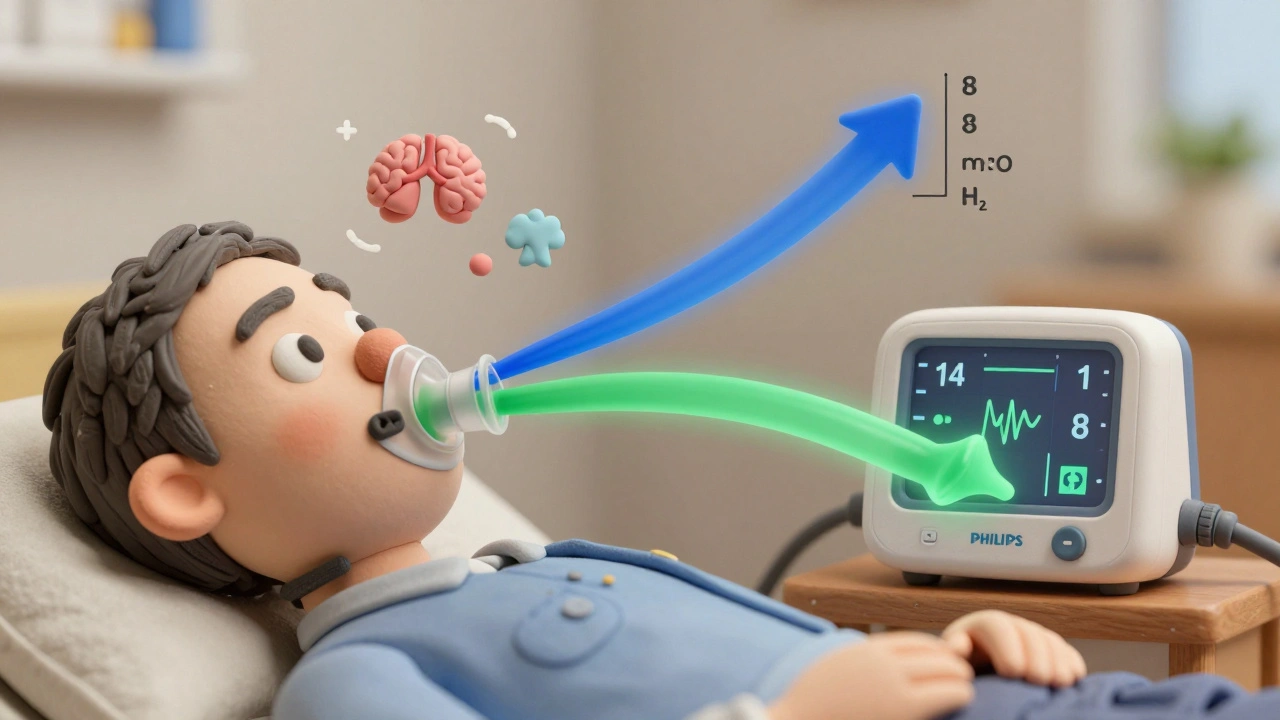
BiPAP-short for Bilevel Positive Airway Pressure-does something different. Instead of one pressure, it gives you two: a higher pressure when you breathe in (called IPAP), and a lower pressure when you breathe out (called EPAP). This difference, often called the pressure swing, can be set anywhere from 3 to 15 cm H₂O.
For example, a BiPAP might be set to 14 cm H₂O when you inhale and 8 cm H₂O when you exhale. That makes breathing out feel easier. If you’ve ever struggled to blow against a constant high pressure, you’ll understand why this matters.
BiPAP machines also have advanced modes. Some can detect if you stop breathing entirely and deliver a breath for you (called a backup rate). This is critical for people with central sleep apnea or neuromuscular diseases, where the brain doesn’t send the right signals to breathe.
BiPAP devices like the Philips DreamStation BiPAP Auto or ResMed AirCurve 10 VAuto are more complex. They’re not just for simple snoring or mild sleep apnea-they’re built for more serious breathing challenges.
When CPAP Is the Best Choice
If you have obstructive sleep apnea (OSA)-the most common type-and no other major lung or heart conditions, CPAP is almost always the first step. It’s cheaper, simpler, and just as effective as BiPAP for most people.
Studies show that CPAP users get the same improvement in sleep quality, daytime alertness, and blood pressure as BiPAP users when their condition is straightforward. One 2021 Cochrane review of nearly 2,000 patients found no meaningful difference in treatment adherence or outcomes between the two for standard OSA.
CPAP is also the go-to for insurance companies. Medicare and most private insurers cover CPAP with minimal paperwork. To get BiPAP approved, you usually have to prove CPAP didn’t work-like if you couldn’t tolerate pressures above 15 cm H₂O for more than a few nights.
Many people start with CPAP and do fine. In fact, a 2023 survey of over 12,000 users found 78% were satisfied with their CPAP therapy, and 62% used it six or more hours a night. That’s the gold standard for success.
When BiPAP Is Necessary
BiPAP isn’t better for everyone. But for certain conditions, it’s the only option that works well.
High CPAP pressure needs: If your doctor prescribes a pressure above 15 cm H₂O, exhaling against that constant force can feel like breathing through a straw. BiPAP’s lower exhalation pressure makes it tolerable. Many patients say switching from CPAP to BiPAP felt like “breathing normally” for the first time in years.
COPD and hypercapnia: If you have chronic obstructive pulmonary disease (COPD) and your blood carries too much carbon dioxide (PaCO₂ >45 mmHg), BiPAP helps your lungs clear out CO₂ more effectively. CPAP alone won’t do this.
Central sleep apnea: This type isn’t caused by a blocked airway-it’s because your brain forgets to tell your body to breathe. BiPAP’s backup rate feature can trigger a breath if you go too long without one. CPAP can’t do that.
Obesity hypoventilation syndrome: People with severe obesity (BMI ≥30) who also have high carbon dioxide levels during the day often need BiPAP. Their bodies struggle to breathe deeply enough, even with airway support.
Neuromuscular diseases: Conditions like ALS, muscular dystrophy, or spinal cord injuries weaken the muscles that control breathing. BiPAP can take over some of that work, especially with timed breathing modes.
Cost and Insurance Differences
CPAP machines cost between $500 and $1,200. BiPAP machines? Usually $800 to $1,800. That’s a big difference, and it matters for insurance.
Medicare and most insurers will cover CPAP right away if your sleep study confirms OSA. But for BiPAP, you typically need to show failure with CPAP first. That means using it for 30 days, at least 4 hours a night, and still being unable to tolerate the pressure. Only then will they approve the more expensive device.
Even if you qualify, BiPAP often comes with higher out-of-pocket costs. Some insurers require prior authorization, additional documentation, or proof from a sleep specialist. Don’t assume BiPAP is automatically covered just because your doctor recommends it.
Real User Experiences
Online forums like Reddit’s r/CPAP are full of stories. One user, u/SleepWarrior2022, wrote: “BiPAP at 14/8 felt like breathing normally. CPAP at 14 felt like choking.” That’s a common theme among people who needed high pressure.
But not everyone has a smooth ride. Some BiPAP users struggle with the machine’s settings. A 2023 survey found 34% of BiPAP users had trouble understanding modes like S/T or Timed, compared to just 18% of CPAP users. Others reported the machine didn’t sync well with their breathing, causing a “cycling” sensation-like the air was pushing and pulling at the wrong times.
CPAP users, on the other hand, tend to praise simplicity. In a 2023 poll, 71% rated CPAP’s ease of use as excellent. For many, that’s the deciding factor.
What Happens After You Get Your Device
Neither device works if you don’t use it. The goal is at least 4 hours a night, 70% of nights, to keep insurance coverage. But most people need time to adjust.
CPAP users usually adapt in 2 to 4 weeks. BiPAP? Often 3 to 6 weeks. Why? Because there’s more to learn. You might need to tweak pressure settings, adjust the ramp feature, or fine-tune the humidity. A respiratory therapist can help, especially with BiPAP. CPAP? Many people figure it out on their own.
Mask fit is the #1 reason people quit. 70% of early discomfort comes from a bad seal. Whether you’re on CPAP or BiPAP, getting the right mask-nasal pillows, full face, or nasal cradle-is just as important as the machine itself.
What’s Next for These Devices
Manufacturers are making both CPAP and BiPAP smarter. ResMed’s AirCurve 10 VAuto uses AI to adjust pressure in real time. Philips’ DreamStation 3 now includes built-in oxygen monitoring. These features help personalize therapy and catch problems early.
But the big question remains: Should BiPAP be used more widely? Some experts, like Dr. Sanjay Patel from Harvard, say yes-for severe OSA with high BMI, BiPAP might improve early adherence. Others, like Dr. David White, argue it’s overused. A 2023 analysis estimated that $420 million is wasted each year in the U.S. on BiPAP for people who only needed CPAP.
The bottom line? BiPAP isn’t a upgrade. It’s a different tool for different problems. Using it for simple sleep apnea doesn’t make you healthier-it just costs more.
How to Decide What’s Right for You
Here’s a quick checklist:
- If you have obstructive sleep apnea and your pressure needs are below 15 cm H₂O → CPAP is your best bet.
- If you need pressure above 15 cm H₂O and can’t tolerate it → ask about BiPAP.
- If you have COPD, heart failure, or high carbon dioxide levels → BiPAP is likely needed.
- If you have central sleep apnea or a neuromuscular disease → BiPAP with backup rate is essential.
- If you’re unsure → get a full sleep study with dual-pressure titration. Don’t guess.
Don’t let price or convenience drive your choice. Use the right tool for your body’s needs. A good night’s sleep isn’t about the machine-it’s about breathing easy.
Can I switch from CPAP to BiPAP if I’m not comfortable?
Yes, but only if your symptoms or pressure needs justify it. If you’re struggling with high CPAP pressure (above 15 cm H₂O), frequent mask leaks, or trouble exhaling, talk to your sleep specialist. They may recommend a follow-up sleep study to test BiPAP settings. Insurance usually requires proof of CPAP failure before approving the switch.
Is BiPAP better for weight loss or improving sleep quality?
No. Neither CPAP nor BiPAP causes weight loss. Both improve sleep quality by stopping breathing pauses. Studies show no difference in sleep quality or daytime fatigue between the two for standard obstructive sleep apnea. The benefit of BiPAP comes from comfort during exhalation-not better sleep.
Do BiPAP machines make more noise than CPAP?
No. Modern BiPAP and CPAP machines are equally quiet. Both use similar motors and sound-dampening technology. The noise level depends on the model-not the type. A ResMed AirSense 11 CPAP and an AirCurve 10 VAuto BiPAP produce nearly identical sound levels. If your machine is loud, check for mask leaks or dirty filters.
Can I use BiPAP if I only have mild sleep apnea?
Technically yes, but it’s not recommended. Mild sleep apnea (AHI 5-14) usually responds well to CPAP at low pressures. BiPAP adds cost and complexity without benefit. Using it unnecessarily can lead to insurance denials, higher out-of-pocket costs, and confusion about your treatment plan. Stick with CPAP unless your doctor has a clear clinical reason for BiPAP.
How often do I need to replace my BiPAP or CPAP machine?
Most insurers cover a new machine every 5 years. Devices typically last 3-7 years with proper care. Signs you need a replacement include louder operation, inconsistent pressure, error messages, or if your therapy data shows poor usage despite good compliance. Always check with your DME provider before replacing-it’s not something you just buy online.
Do I need a prescription for CPAP or BiPAP?
Yes. Both are Class II medical devices regulated by the FDA. You need a sleep study and a doctor’s prescription to get either machine. Even if you buy one online, you’ll need to submit your prescription to your insurance or supplier. Never use a device without proper titration-it can be dangerous.

