Why Antibiotic Allergy Testing Matters
Many people believe they’re allergic to penicillin or other antibiotics because they had a rash, nausea, or dizziness years ago. But here’s the truth: over 90% of people who think they’re allergic to penicillin aren’t. That’s not a guess-it’s backed by data from the CDC and major medical societies. When you carry an unconfirmed allergy label, doctors avoid using the safest, cheapest, and most effective antibiotics. Instead, they turn to broader-spectrum drugs that cost more, cause more side effects, and fuel antibiotic resistance.
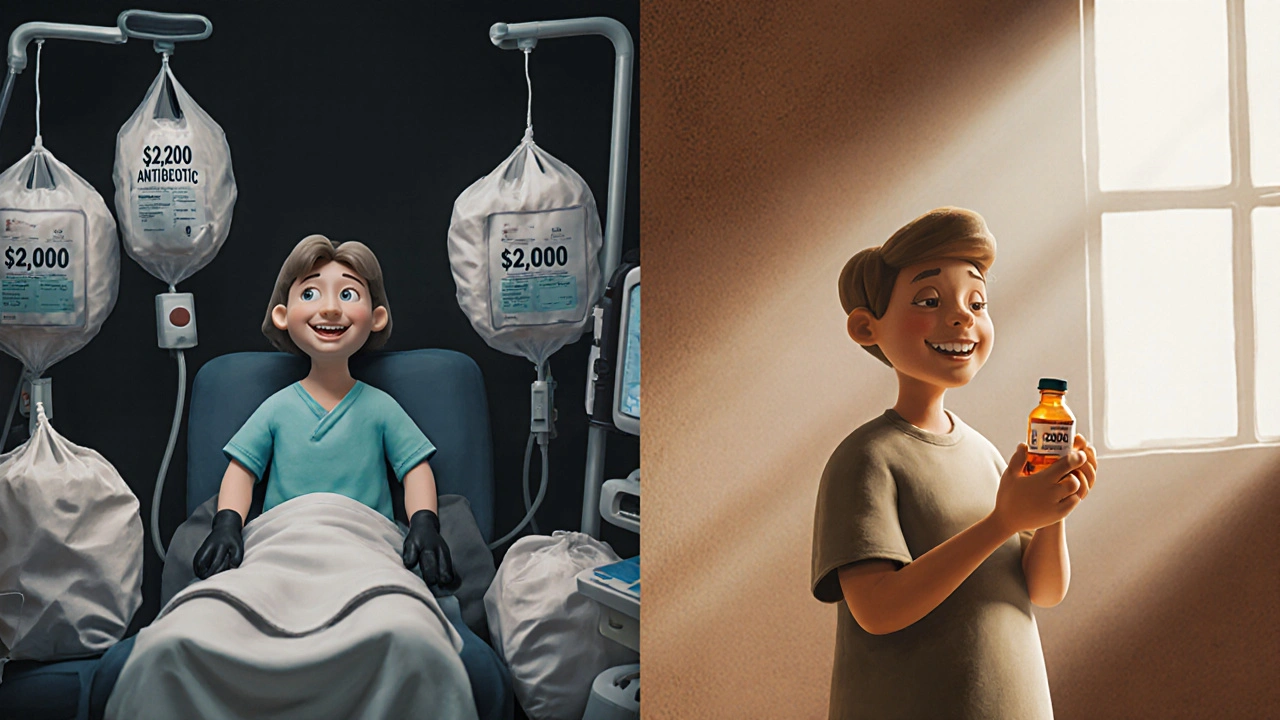
Testing isn’t just about avoiding a rash. It’s about getting the right treatment when you’re sick. A confirmed non-allergy can mean switching from a $2,000 IV antibiotic to a $12 pill. It can mean fewer hospital days, fewer complications, and less risk of superinfections like C. diff. If you’ve ever been told you’re allergic to penicillin-or any antibiotic-testing could change how you’re treated for the rest of your life.
What You Need to Stop Taking Before Testing
Antibiotic allergy testing relies on your body’s real-time reaction to small doses of the drug. If you’re taking certain medications, your body won’t react the way it should-and the test will be useless. This part is non-negotiable.
First, stop all first-generation antihistamines like diphenhydramine (Benadryl) and hydroxyzine. You need to stop these at least 72 hours before your appointment. These are common in sleep aids, cold meds, and allergy pills. Check the labels.
Second, stop second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra), and levocetirizine (Xyzal). These last longer in your system. You need to stop them seven full days before testing. Even one dose can interfere.
Third, if you take tricyclic antidepressants like doxepin, you must stop them 14 days before testing. These also block histamine and can mask reactions. Don’t stop these on your own-talk to your doctor first. If you’re on blood pressure meds like ACE inhibitors, tell your allergist. They don’t need to be stopped, but they can make anaphylaxis harder to treat if it happens.
Keep taking everything else: heart meds, asthma inhalers, thyroid pills, insulin. Don’t stop anything unless your allergist says so. Missing a dose of your essential meds is riskier than any test.
What Happens During the Test
Antibiotic allergy testing isn’t one thing-it’s a step-by-step process designed to be safe and accurate. It usually takes 2 to 3 hours, and you’ll be monitored the whole time.
Step one is the skin prick test. A tiny drop of penicillin solution is placed on your skin, then lightly pricked with a plastic device. It feels like a quick mosquito bite. No needles. No pain. If your skin turns red, itchy, and swells more than 3mm, that’s a positive sign. If nothing happens, you move to the next step.
Step two is the intradermal test. A small amount of the antibiotic is injected just under the skin with a thin needle. You’ll see a small bump, like a mosquito bite. After 15 minutes, the doctor checks for swelling or redness. This step is more sensitive than the skin prick and catches reactions the first test might miss.
Step three is the oral challenge. If both skin tests are negative, you’ll take a small dose of the antibiotic-usually 10% of a regular pill. You’ll wait 30 minutes. If you’re fine, you’ll take the full dose and wait another 60 minutes. You’re watched closely during this time. You might feel nervous, but most people say it’s easier than they expected. One patient described it as “just swallowing a regular pill.”
What a Positive or Negative Result Means
A positive skin test means your immune system reacted to the antibiotic. That’s strong evidence you’re truly allergic. The chance of a false positive is less than 2%. If you test positive, you’ll avoid that drug and likely be given alternatives.
A negative result means you’re not allergic-not just “probably not.” The negative predictive value is 95-98%. That means if you test negative, you’re almost certainly safe to take the antibiotic. This is called “de-labeling.” You’ll get a letter from your allergist to give to your doctor. Your medical record will be updated. No more “penicillin allergy” on your chart.
But here’s something many don’t know: allergies can fade. If you had a reaction 10 years ago, there’s an 80% chance you’ve outgrown it. That’s why retesting is so valuable-even if you were told you were allergic decades ago, testing now could change your future care.
What to Expect After the Test
Most people feel fine right after. But some reactions show up later.
Within a few hours, you might notice mild itching or redness at the test site. That’s normal. You can use hydrocortisone cream if it bothers you. About 15% of people get this delayed reaction.
Some people feel a little anxious, dizzy, or nauseous after the oral challenge. That’s not always an allergy. Anxiety can mimic symptoms. Your doctor will help you tell the difference. If you had a true reaction, you’d get hives, trouble breathing, or swelling-signs they’re watching for during the test.
After the test, you can drive, eat, and go back to work. No recovery time. No restrictions. Just peace of mind.
Why This Test Is Worth the Effort
Every dollar spent on testing saves $5.70 in future healthcare costs. That’s not theory-it’s a published study. Patients who get de-labeled use fewer broad-spectrum antibiotics. They have fewer infections. They leave the hospital sooner. Their bills drop.
One patient in a 2023 study switched from daptomycin ($1,850 per dose) to penicillin ($12 per dose) after testing. His annual antibiotic cost dropped from $67,525 to $4,380. That’s not rare. It’s common.
And it’s not just about money. It’s about access. If you’re allergic to penicillin, you might be denied antibiotics that work best for your infection. If you’re not allergic, you’re not getting the right care. Testing fixes that.
Where to Get Tested
Not every clinic can do this. You need an allergist trained in drug testing. Most hospitals and university medical centers have allergy departments that specialize in this. Primary care doctors can’t do it-they don’t have the equipment or the training.
If you live in a rural area, you might need to travel. But that’s changing. New pilot programs are testing at-home challenges under telemedicine supervision. Early results show 95% success. It’s not available everywhere yet, but it’s coming.
Ask your doctor for a referral to an allergist who does antibiotic testing. Don’t wait for a hospital stay to find out you’re not allergic. Get tested now-before you need antibiotics again.
Common Myths About Antibiotic Allergy Testing
Myth: Blood tests can confirm antibiotic allergies. False. Blood tests for penicillin allergy are unreliable. They’re not used in clinical practice. Skin testing is the gold standard.
Myth: If I had a reaction once, I’ll always be allergic. False. Most people lose their allergy over time. Retesting is safe and recommended.
Myth: The test is dangerous. False. The risk of a severe reaction during testing is 0.06%. That’s lower than the risk of a bee sting. Epinephrine is always on hand. The test is safer than taking the wrong antibiotic.
Myth: I don’t need to test if I never take penicillin. False. You might need it someday. A simple infection, a surgery, a pregnancy-any of these could require penicillin. Being labeled allergic limits your options forever.
Final Thoughts
Antibiotic allergy testing isn’t complicated. It’s not painful. It doesn’t take long. But it changes everything. If you’ve ever been told you’re allergic to penicillin-or any antibiotic-ask for a referral to an allergist. Get tested. Your future self will thank you.

