Most people don’t realize that generic medications are just as safe and effective as brand-name drugs-yet many still hesitate to take them. If you’ve ever looked at your prescription and thought, ‘Will this really work the same?’, you’re not alone. The truth is, 9 out of 10 prescriptions in the U.S. are filled with generics. They save patients billions each year and work just like their brand-name counterparts. But if your doctor doesn’t bring it up, or if you’re unsure how to ask, you might miss out on affordable, proven treatment.
Why generics are not second-rate
Generic drugs aren’t cheap imitations. They contain the exact same active ingredient, in the same strength and dosage form, as the brand-name version. The U.S. Food and Drug Administration (FDA) requires them to meet the same strict standards for quality, purity, and stability. Every generic must prove it delivers the same amount of medicine into your bloodstream at the same rate as the brand-name drug-within a tight 80-125% range. That’s not guesswork. It’s science.Many people assume generics are made in lower-quality factories. That’s not true. The same FDA inspections apply to both brand and generic manufacturers. In fact, many brand-name companies actually make their own generic versions. The FDA inspected over 3,500 facilities worldwide in 2023, and 98.7% passed. If a factory can’t meet the standards, it doesn’t get approved-no matter if it’s making Lipitor or its generic version, atorvastatin.
What’s different about generics-and what’s not
The only real differences between a generic and a brand-name drug are the inactive ingredients: fillers, dyes, and coatings. These don’t affect how the medicine works. They just change the pill’s color, shape, or taste. That’s why your generic might look completely different from the brand you used to take. But that’s like switching from a red sports car to a blue one-the engine is still the same.Some patients worry these inactive ingredients cause side effects. While rare, about 0.8% of reported concerns relate to this. For most people, switching to a generic causes no change at all. In fact, a 2020 study in JAMA Internal Medicine looked at 47 clinical trials involving heart medications and found no meaningful difference in effectiveness between generics and brands. Patients who switched to generics saved an average of $2,847 per year.
Why patients still hesitate
The biggest reason people avoid generics isn’t science-it’s perception. A 2022 survey found that 68% of patients believe cheaper means worse. Another 52% distrust manufacturing quality, especially if the drug comes from overseas. And 47% just don’t trust the system.These beliefs are understandable. You’ve seen ads telling you brand-name drugs are ‘superior.’ You’ve heard stories online about someone who felt ‘off’ after switching. But here’s what those stories don’t tell you: in a 2023 survey of 12,500 patients, 79% said they noticed no difference in effectiveness after switching to generics. And 68% said they requested generics specifically because they couldn’t afford the brand.
One exception exists: drugs with a narrow therapeutic index, like levothyroxine (for thyroid conditions) or warfarin (a blood thinner). These require very precise dosing. Even small changes in how the drug is absorbed can matter. That’s why the FDA applies stricter bioequivalence rules for these-within 90-110% instead of 80-125%. If you take one of these, your doctor will monitor you closely after switching. But even here, most patients do just fine.

How to start the conversation
You don’t need to be an expert to ask smart questions. Here’s a simple way to bring it up:- Ask: ‘Is there a generic version of this medication?’
- Tell: ‘I’d like to use it if it’s just as safe and effective.’
- Ask again: ‘Can you explain how it works the same way?’
This is called the ‘Ask-Tell-Ask’ method. It’s used by top health systems because it works. A 2022 study showed it cuts medication errors by 37%. It also helps your doctor understand your concerns instead of assuming you’re just trying to save money.
If your doctor says no, ask why. Is it because of your condition? Is it because the generic isn’t available? Or is it just habit? If they say, ‘The brand is better,’ ask for evidence. The FDA, the American Medical Association, and major medical journals all agree: for most drugs, there’s no clinical difference.
What to do if you’ve had a bad experience
If you switched to a generic and felt worse, don’t assume it’s the drug’s fault. But don’t ignore it either. Some people are sensitive to changes in inactive ingredients-especially with thyroid meds or seizure drugs. If you notice new side effects, contact your doctor or pharmacist right away. They can switch you back or try a different generic manufacturer.There are over 15,000 generic drugs approved in the U.S., made by hundreds of companies. One manufacturer’s version might suit you better than another’s. Your pharmacist can help you find the right one. Many pharmacies even let you request a specific generic brand if you’ve had success with it before.
Cost matters-especially with chronic conditions
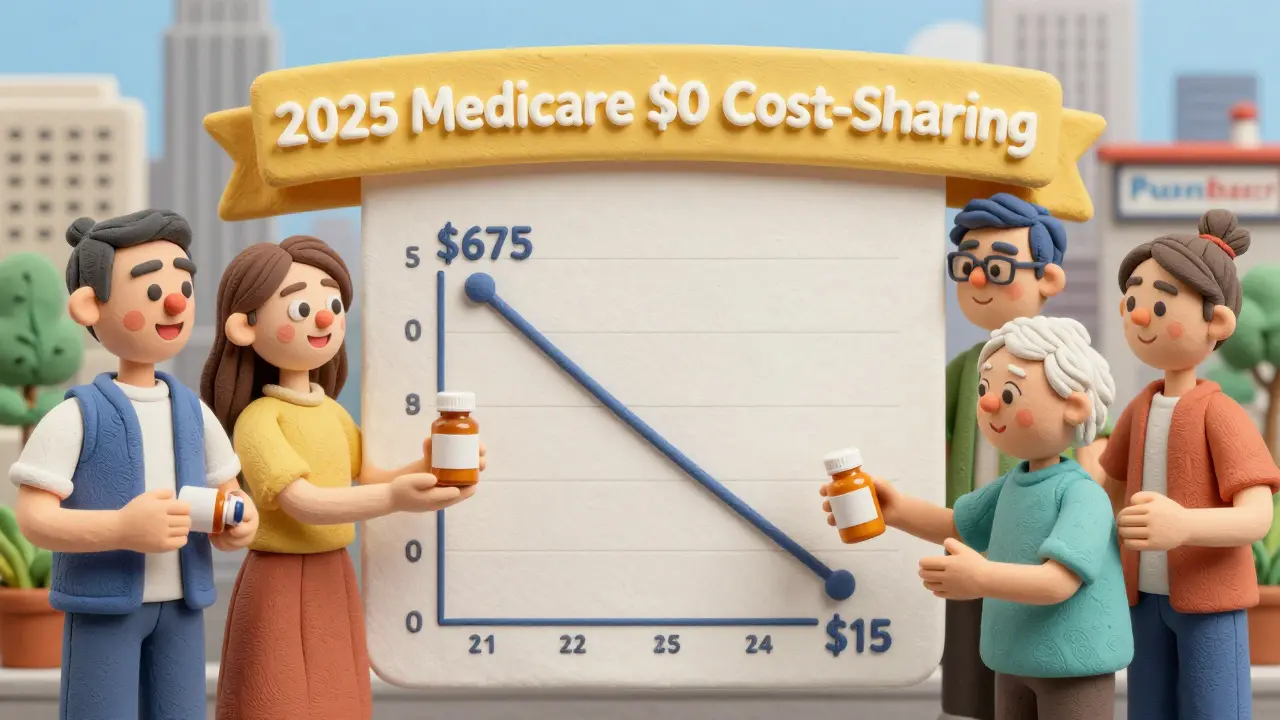
For people managing diabetes, high blood pressure, or high cholesterol, cost is a daily reality. A 2023 IQVIA report showed the average cost of a generic prescription is $15.78. The brand-name version? $674.89. That’s not a typo. That’s over 97% less.Studies show patients on generics for chronic conditions are 8-12% more likely to keep taking their meds. Why? Because they can afford them. Skipping doses because of cost is one of the biggest reasons people end up in the hospital. Generics help prevent that.
Starting in 2025, Medicare Part D will cover many generics with $0 cost-sharing. That means if you’re on Medicare, you could soon be paying nothing for your heart or diabetes meds. But you won’t get that benefit unless you ask for the generic.
What your pharmacist can do
Your pharmacist is trained to explain generics. They see hundreds of patients every week who have the same questions. In fact, 47% of all pharmacy inquiries are about whether generics work as well as brand-name drugs. Pharmacists resolve 83% of those concerns with simple, clear answers.Don’t just pick up your prescription and leave. Ask: ‘Can you tell me what’s in this pill?’ or ‘Is this the same as the brand?’ They can show you the FDA-approved Medication Guide that comes with it. They can also tell you which generic manufacturer made it-something you can track if you ever have a reaction.
What to do next
If you’re taking a chronic medication, check your next prescription. Is it brand or generic? If it’s brand, ask your doctor or pharmacist if a generic is available. If you’re starting a new medication, ask upfront. Don’t wait until the bill arrives.Don’t let myths keep you from affordable care. Generics aren’t a compromise-they’re a smart choice backed by decades of science, millions of patients, and strict government oversight. The only thing that changes when you switch is the price. The effectiveness? It stays exactly the same.
Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence-meaning they deliver the same amount of medicine into your bloodstream at the same rate. A 2020 study of 47 clinical trials found no meaningful difference in effectiveness for cardiovascular drugs. Generics are not cheaper because they’re weaker-they’re cheaper because they don’t require repeating expensive clinical trials.
Why do generic pills look different from brand-name pills?
The difference in color, shape, or size comes from inactive ingredients-like dyes or fillers-that don’t affect how the medicine works. By law, generic manufacturers can’t copy the exact appearance of brand-name pills to avoid trademark issues. But the active ingredient is identical. These changes are cosmetic, not medical.
Can inactive ingredients in generics cause side effects?
Rarely. About 0.8% of patient concerns relate to inactive ingredients. Some people may be sensitive to certain dyes or fillers-like lactose or gluten-but these are listed on the Medication Guide. If you have known allergies or sensitivities, talk to your pharmacist. For most people, switching to a generic causes no side effects. In fact, 79% of patients in a 2023 survey reported no difference in how they felt after switching.
Are generics made in unsafe factories?
No. The FDA inspects all manufacturing facilities-whether they make brand or generic drugs-with the same standards. In 2023, 98.7% of generic drug facilities passed inspection. Many brand-name companies even produce their own generics. The FDA doesn’t distinguish between countries of origin; it only checks if the facility meets U.S. safety rules. If a factory fails, it’s shut down-regardless of who owns it.
Should I avoid generics for thyroid or blood thinner medications?
Not necessarily. For drugs like levothyroxine or warfarin, the FDA requires tighter bioequivalence standards (90-110% instead of 80-125%) because small changes can matter. If you switch, your doctor may check your blood levels more often at first. But most patients adjust without issue. The key is consistency: once you start a specific generic, stick with it. Don’t keep switching between brands unless your doctor advises it.
Will my insurance cover generics?
Almost always-and at a much lower cost. Most insurance plans require you to try the generic first. If the brand is prescribed without a generic alternative, you’ll pay more. Starting in 2025, Medicare Part D will cover many generics with $0 cost-sharing. Even without insurance, generics typically cost under $20 per prescription, while brand-name versions can be hundreds.
What if I don’t like how the generic makes me feel?
Contact your doctor or pharmacist. While most people feel no difference, a small number may respond differently to inactive ingredients or slight variations in absorption. Your provider can switch you back to the brand or try a different generic manufacturer. Keep track of when symptoms started and what changes occurred. This helps your provider make the best decision.
Can I ask for a specific generic brand?
Yes. Pharmacists can often fill your prescription with a specific generic manufacturer if you’ve had success with it before. Just ask: ‘Can you get me the same generic I took last time?’ Some pharmacies even let you choose based on price or availability. If your insurance requires a specific one, they’ll let you know.

