When placenta previa occurs, the placenta covers part or all of the cervix, making vaginal delivery dangerous. The biggest risk isn’t the position itself-it’s the massive bleeding that can happen during labor or after delivery. In many cases, doctors plan a C-section to avoid this. But what if bleeding starts before surgery? Or if you’re in a remote area without immediate surgical access? That’s where misoprostol comes in.
What Is Misoprostol and How Does It Work?
Misoprostol is a synthetic version of prostaglandin E1, a natural substance your body makes to trigger contractions. It’s been used for decades to induce labor, prevent postpartum bleeding, and even for medical abortions. But its role in placenta previa is different-it’s not about starting labor. It’s about stopping life-threatening bleeding.
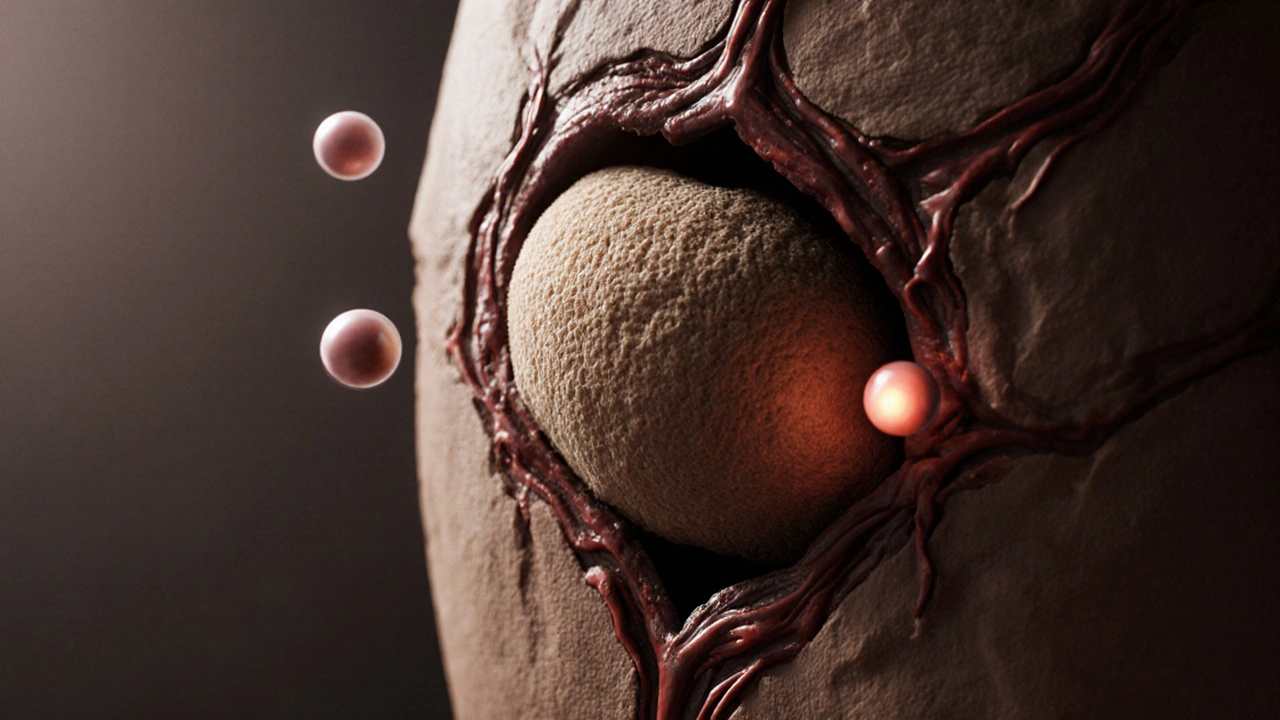
When the placenta is stuck low in the uterus, the uterine muscles can’t contract properly around it. Think of it like trying to squeeze a sponge that’s still attached to the wall-the blood vessels stay open, and bleeding doesn’t stop. Misoprostol forces those muscles to clamp down hard, even where the placenta is stuck. This reduces blood flow dramatically, buying critical time.
Why Not Just Use Oxytocin?
Oxytocin is the first-line drug for postpartum hemorrhage. It’s fast, effective, and widely available. But in placenta previa, it often doesn’t work well. Why? Because the placenta physically blocks the lower uterine segment-the very area where oxytocin needs to act. The muscle above the placenta contracts, but the area around the placenta stays relaxed. Blood keeps flowing.
Misoprostol works differently. It’s absorbed through the lining of the mouth, rectum, or vagina, and reaches the entire uterus evenly. It doesn’t rely on the placenta being in a certain spot. That’s why it’s become a go-to option in emergencies, especially where IV drugs and skilled staff aren’t immediately available.
How Is It Given in Placenta Previa Cases?
The most common route is sublingual-putting 600 micrograms (three 200 mcg tablets) under the tongue. This lets the drug absorb quickly through the mucous membranes. Within 15 to 30 minutes, contractions start, and bleeding slows. Some providers use the vaginal route, especially if the patient is already in labor. Rectal use is less common but still effective.
A 2021 study in the International Journal of Gynecology & Obstetrics tracked 147 women with placenta previa and major bleeding. Those given sublingual misoprostol saw bleeding stop in under 20 minutes in 82% of cases. Only 12% needed emergency surgery after treatment. That’s a huge improvement compared to using oxytocin alone.
When Is It Used-and When Is It Not?
Misoprostol isn’t a cure for placenta previa. It’s a bridge. You still need a C-section eventually. But it can turn a crisis into a manageable situation.
It’s most useful when:
- Bleeding starts before a planned C-section
- The hospital is far from a surgical center
- IV oxytocin isn’t working
- There’s no blood bank or anesthesiologist on standby
It’s not recommended if:
- The patient has asthma or a history of severe allergic reactions to prostaglandins
- There’s a known uterine scar from prior C-section or myomectomy (higher risk of rupture)
- The patient is already in active labor with fetal distress
Doctors always weigh the risks. A ruptured uterus is rare with misoprostol-but it’s serious. That’s why it’s not used lightly, even in emergencies.

Side Effects and What to Watch For
Misoprostol isn’t gentle. It causes strong contractions. That’s the point-but it also means side effects are common.
Most women get:
- Shivering and fever (up to 70% of cases)
- Nausea and vomiting
- Diarrhea
- Headache
These usually fade within 2 hours. Fever over 38.5°C (101.3°F) is common and doesn’t always mean infection. But if it lasts longer than 4 hours or comes with chills and confusion, it needs checking.
More serious risks include:
- Uterine hyperstimulation-contractions too close together, risking fetal distress
- Uterine rupture-rare, but more likely if the patient has had prior surgery
- Severe hypotension (low blood pressure)
That’s why misoprostol should never be given without monitoring. Even in remote settings, someone needs to check the mother’s pulse, blood pressure, and contractions every 15 minutes after giving the drug.
Real-World Use in Low-Resource Settings
In rural Nigeria, Ethiopia, and parts of India, misoprostol has saved lives where no one has ever seen a C-section. In one 2023 field trial in rural Uganda, health workers trained in misoprostol use reduced maternal deaths from placenta previa by 63% over 18 months. They kept the tablets in cool, dry boxes and taught midwives to recognize bleeding early.
The drug’s stability is a huge advantage. Unlike oxytocin, which needs refrigeration, misoprostol lasts for years at room temperature. It doesn’t need needles, IV lines, or electricity. That’s why WHO recommends it as part of emergency obstetric kits in low-resource areas.
What Comes After Misoprostol?
Stopping the bleeding is only the first step. Once bleeding slows, the team prepares for delivery. Even if the mother feels stable, placenta previa doesn’t fix itself. The placenta is still stuck. It won’t detach safely on its own.
After misoprostol, the next steps are:
- Transfer to a facility with surgical capabilities as soon as possible
- Start IV fluids and crossmatch blood
- Monitor fetal heart rate continuously
- Prepare for possible hysterectomy if placenta is deeply attached (placenta accreta)
Some women who get misoprostol end up needing a C-section within 2 hours. Others wait 12-24 hours. The goal isn’t speed-it’s safety. Misoprostol gives you that window.
Alternatives and When to Consider Them
Misoprostol isn’t the only option. In hospitals with good resources, doctors might use:
- Carboprost (Hemabate): A stronger prostaglandin, given by injection. More effective but more side effects-severe cramping, diarrhea, high fever.
- Methylergonovine: Works fast but can raise blood pressure. Not safe for women with preeclampsia or heart disease.
- Bakri balloon: A tamponade device inserted into the uterus to compress bleeding. Requires surgery and skilled staff.
Misoprostol wins on accessibility, cost, and ease of use. It costs less than $1 per dose. Carboprost can be over $20. That’s why it’s the drug of choice outside big hospitals.
Final Thoughts: A Lifesaving Tool, Not a Magic Bullet
Misoprostol doesn’t make placenta previa disappear. It doesn’t replace surgery. But in the minutes before a C-section, when every second counts, it can mean the difference between life and death. It’s not glamorous. It’s not high-tech. But it’s reliable, cheap, and works when nothing else does.
For women in remote areas, or for emergency teams rushing to a hospital, misoprostol is one of the few tools that actually gives them control. It’s not perfect. But in obstetrics, where perfection is rare, sometimes the best thing you can do is have something that works-when you need it most.
Can misoprostol be used to induce labor in placenta previa?
No. Misoprostol should never be used to start labor in placenta previa. Inducing labor increases the risk of sudden, massive bleeding. The goal with misoprostol in this situation is to stop bleeding, not to start contractions for delivery. Labor should only be induced after the placenta has been safely removed via C-section.
Is misoprostol safe if I’ve had a previous C-section?
It’s risky. Women with a prior C-section have a higher chance of uterine rupture when given misoprostol, especially at higher doses. If bleeding occurs and a C-section isn’t immediately possible, doctors may still use a lower dose (200-400 mcg) under strict monitoring-but only as a last resort. The risk must be weighed against the danger of uncontrolled bleeding.
How long does misoprostol take to stop bleeding in placenta previa?
Most women see reduced bleeding within 15 to 30 minutes after taking misoprostol sublingually. Complete control often happens within 45 minutes. If bleeding continues past an hour, other interventions like surgery or a Bakri balloon are needed immediately.
Can I take misoprostol at home if I have placenta previa?
Absolutely not. Placenta previa is a medical emergency. Even though misoprostol is available over the counter in some countries, using it without medical supervision can lead to uterine rupture, fetal death, or uncontrolled hemorrhage. Always seek emergency care immediately if you have vaginal bleeding during pregnancy.
Does misoprostol affect future pregnancies?
There’s no evidence that a single dose of misoprostol for postpartum bleeding affects future fertility or increases the risk of placenta previa in later pregnancies. The drug is metabolized and cleared from the body within hours. However, any major obstetric event-including severe bleeding-can impact future pregnancy outcomes. Close monitoring in future pregnancies is recommended.
What to Do If You’re at Risk
If you’ve been diagnosed with placenta previa, don’t wait for bleeding to start. Talk to your provider about your emergency plan. Ask:
- Where’s the nearest hospital with a C-section capability?
- Do they stock misoprostol for emergencies?
- What signs should I watch for that mean I need to go in right away?
- Do I need to carry a medical alert card?
Many women with placenta previa go full term without bleeding. But for those who do, having a plan can save your life. Misoprostol isn’t a substitute for care-it’s a tool that makes care possible when time is running out.

