Penile Surgery for Prosthesis Complications: When and How
Explore when and how penile surgery addresses prosthesis complications like infection, erosion, and mechanical failure, with clear steps, approaches, and post‑op care.
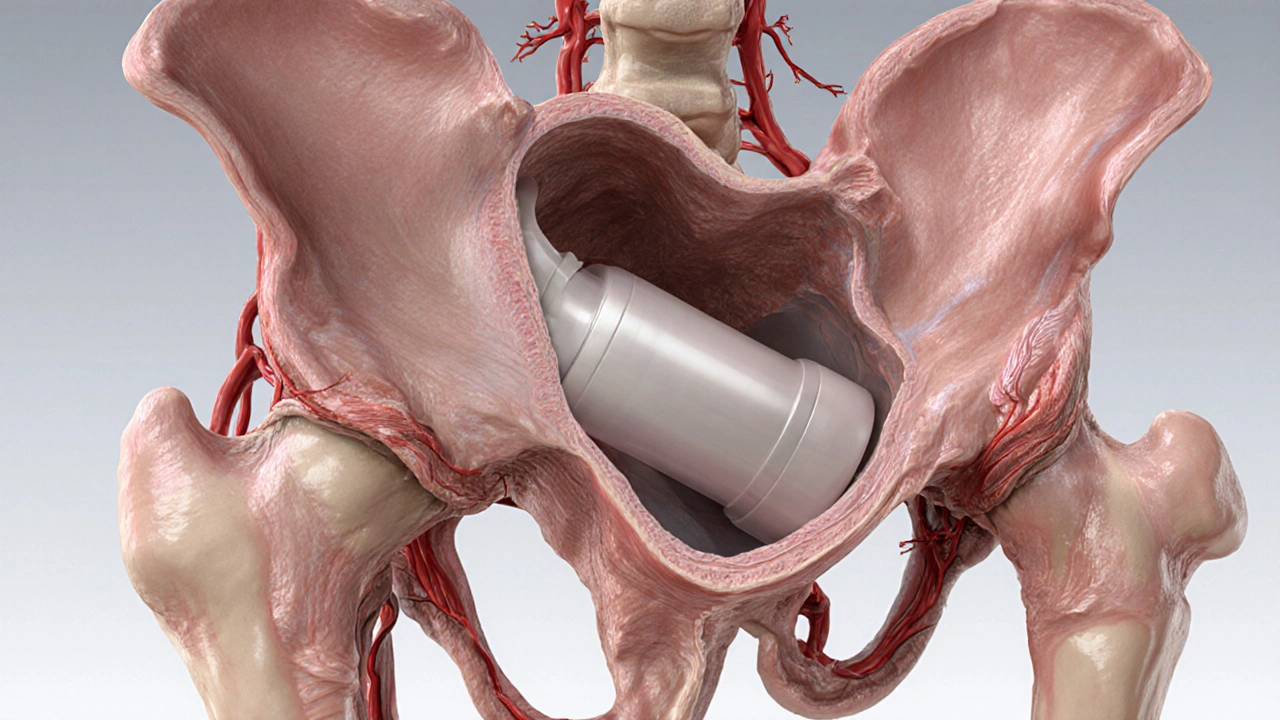
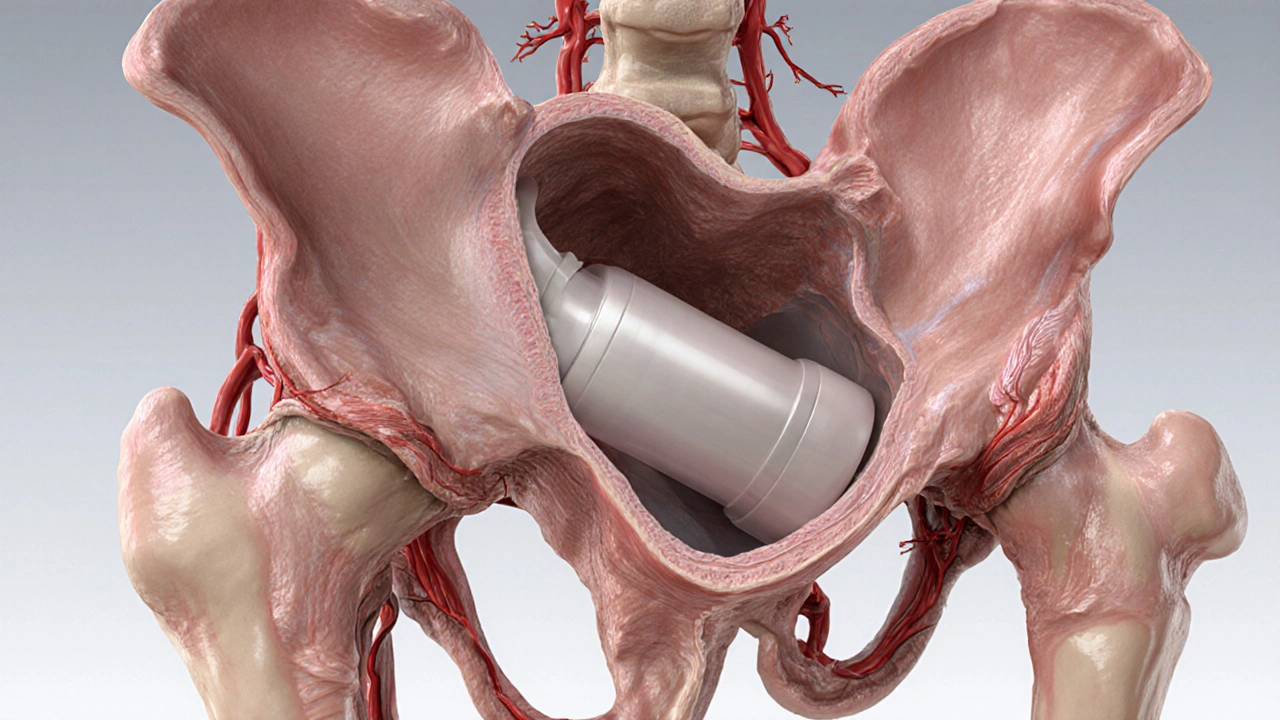
When dealing with prosthesis infection, an infection that develops on or around an implanted medical device such as a joint replacement. It’s also known as prosthetic joint infection and frequently involves a stubborn biofilm, a protective matrix that shelters bacteria from the immune system and antibiotics.
Most infections are caused by bacteria that are already living on the skin. Staphylococcus aureus tops the list, followed closely by coagulase‑negative staphylococci like S. epidermidis. Gram‑negative rods such as Pseudomonas and even fungi can slip in, especially in patients with weakened immunity or prolonged surgical times. The organism type dictates not only the severity of the infection but also the choice of drugs and the need for surgical intervention.
Clinically, infections fall into three time frames. Early infections appear within the first month after surgery and often present with pain, swelling, and fever. Delayed infections show up between one and twelve months, usually with subtle pain and occasional drainage. Late infections, occurring after a year, may mimic aseptic loosening and can be tricky to spot. Diagnosis relies on a combination of laboratory and imaging clues. Elevated C‑reactive protein (CRP) and erythrocyte sedimentation rate (ESR) raise suspicion, while joint aspiration provides definitive cultures. Advanced imaging, especially diagnostic imaging such as MRI with metal‑artifact reduction or nuclear scans, helps locate the infection and assess bone involvement.
Treating a prosthesis infection usually means tackling both the bacteria and the hardware. Surgical debridement, often combined with exchange of modular components, removes the bulk of infected tissue and disrupts the biofilm. When debridement alone isn’t enough, a two‑stage revision—removing the implant, inserting an antibiotic‑laden spacer, and re‑implanting once cultures are clear—offers the highest success rate. Parallel to surgery, antibiotic therapy must be tailored to the organism’s sensitivities, delivered intravenously for several weeks, and then switched to oral agents for a prolonged course. Rifampin, for example, penetrates biofilm well and is often added for staphylococcal infections.
Prevention starts before the patient even steps into the operating room. Pre‑operative skin decolonization with chlorhexidine, optimized glycemic control, and appropriate timing of prophylactic antibiotics (typically a first‑generation cephalosporin given within 60 minutes of incision) cut the bacterial load dramatically. Intra‑operative measures like laminar airflow, proper glove changes, and the use of antimicrobial‑impregnated cement add extra layers of protection. Post‑operative wound care, early mobilization, and patient education on signs of infection keep the risk low once the surgical site is closed.
Even after successful eradication, close follow‑up is essential. Regular monitoring of inflammatory markers, periodic radiographs, and a low threshold for re‑aspiration when symptoms reappear help catch a recurrence early. Physical therapy should balance protecting the new joint while restoring function, and patients should be counseled on lifestyle factors—such as smoking cessation and weight management—that influence long‑term implant survival.
In short, a prosthesis infection is a battle against biofilm‑protected microbes, requiring precise diagnosis, aggressive surgical cleanup, and customized antibiotic regimens. Understanding the pathogen profile, using targeted diagnostic imaging, and following strict preventive protocols form the backbone of successful outcomes. Whether you’re a patient gearing up for joint replacement or a clinician planning a revision, recognizing these core elements can make the difference between a quick recovery and a chronic problem.
Below you’ll find a curated list of articles that dive deeper into each of these topics— from choosing the right antibiotic to mastering surgical techniques—so you can explore the details that matter most to your situation.
Explore when and how penile surgery addresses prosthesis complications like infection, erosion, and mechanical failure, with clear steps, approaches, and post‑op care.