Penile Prosthesis Complication Assessment Tool
Assessment Parameters
Select the symptoms and conditions that apply to your situation to determine if surgical intervention is likely necessary.
Surgical Intervention Recommendation
Quick Takeaways
- Most prosthesis issues-infection, erosion, or mechanical failure-can be addressed surgically before removing the device.
- Choosing the right surgical route (scrotal, perineal, or combined) depends on the complication type, tissue quality, and patient health.
- Early intervention, proper antibiotics, and meticulous technique cut re‑operation rates by up to 30%.
- Revision surgery preserves penile length and sensation when performed by an experienced surgeon.
- Post‑op protocols now favor early mobilisation and a 24‑hour drain‑free approach for most patients.
Complications after a penile prosthesis are rare, but when they happen they can be distressing. Understanding which problems call for a secondary surgery-and what that surgery looks like-helps patients and surgeons avoid unnecessary explantation.
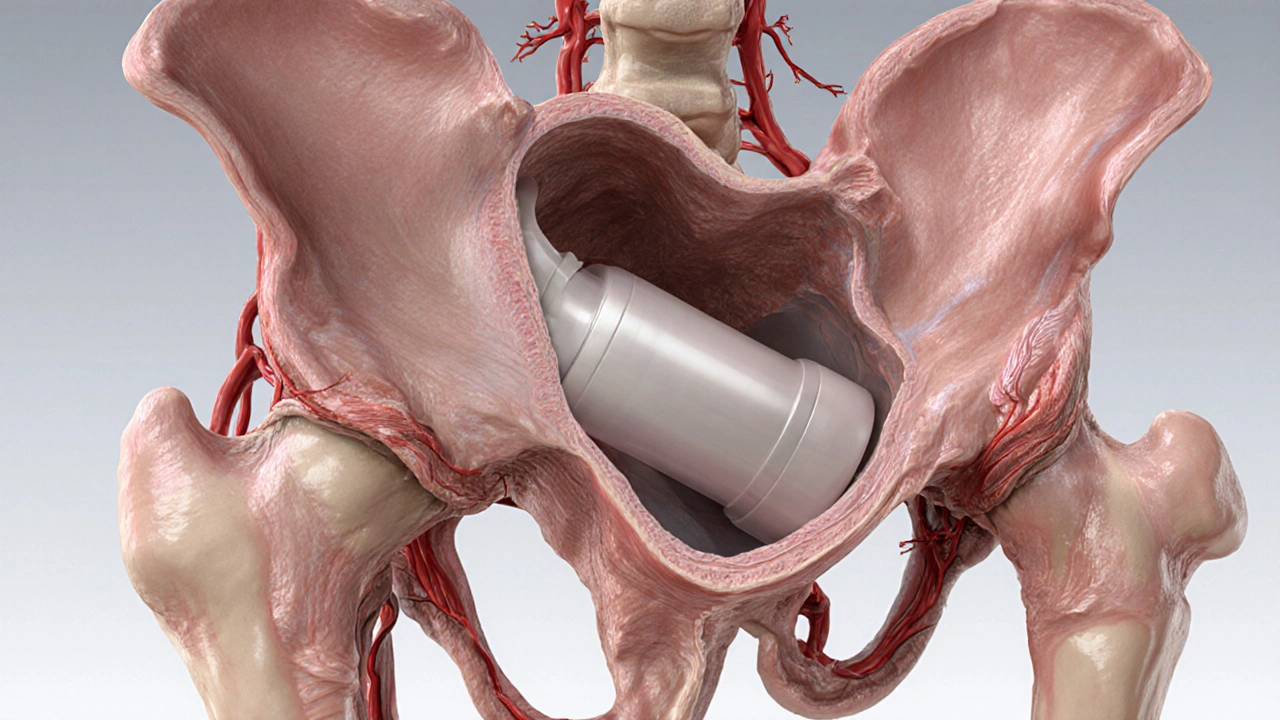
Penile prosthesis is a medical device implanted into the corpora cavernosa to enable an erection for men with severe erectile dysfunction. While modern inflatable and semi‑rigid models have failure rates below 5% over five years, issues such as infection, erosion, mechanical malfunction, and corporal fibrosis still occur. When conservative measures fail, penile surgery becomes the mainstay for salvaging the implant or restoring function.
Why Surgery Becomes Necessary
Not every complication warrants a trip to the operating theatre. The decision hinges on three factors:
- Severity of the problem - A mild mechanical hiccup may be fixed in‑office with a pressure‑adjustment kit, whereas a deep‑seated infection demands debridement.
- Tissue health - Scarring, fibrosis, or ulceration limits the surgeon’s ability to place new cylinders safely.
- Patient comorbidities - Diabetes, immunosuppression, or poor wound‑healing raise the risk of postoperative infection.
When any of these thresholds are crossed, the goals of surgery shift to:
- Eradicating infection or removing damaged tissue.
- Preserving as much penile length and sensation as possible.
- Preparing a clean field for a potential revision implant.
Common Prosthesis Complications Requiring Surgical Intervention
- Prosthesis infection - Often presents with redness, swelling, fever, or drainage. Cultures guide targeted antibiotics.
- Prosthesis erosion - The device presses through the tunica albuginea, sometimes creating a urethral fistula.
- Mechanical failure - Pump leakage, cylinder rupture, or tubing breakage that prevents inflation.
- Corporal fibrosis - Excess scar tissue limits cylinder expansion and can cause painful erections.
- Explanted or abandoned device - Rare, but some men keep a non‑functional prosthesis in situ to avoid repeated surgeries.
Surgical Options: From Explantation to Revision
There are three core pathways:
- Device explantation only - Complete removal with no immediate replacement. Used when infection is uncontrolled or tissue damage is severe.
- Immediate explant‑and‑replace - Removal of the infected or damaged implant followed by a fresh prosthesis in the same session. Success hinges on aggressive intra‑operative antibiotics and meticulous debridement.
- Staged revision - First operation clears infection and allows tissue recovery (usually 3‑6months). The second stage implants a new device.
Choosing among these strategies depends on the organism involved, the extent of tissue loss, and the patient’s willingness to tolerate a second procedure.
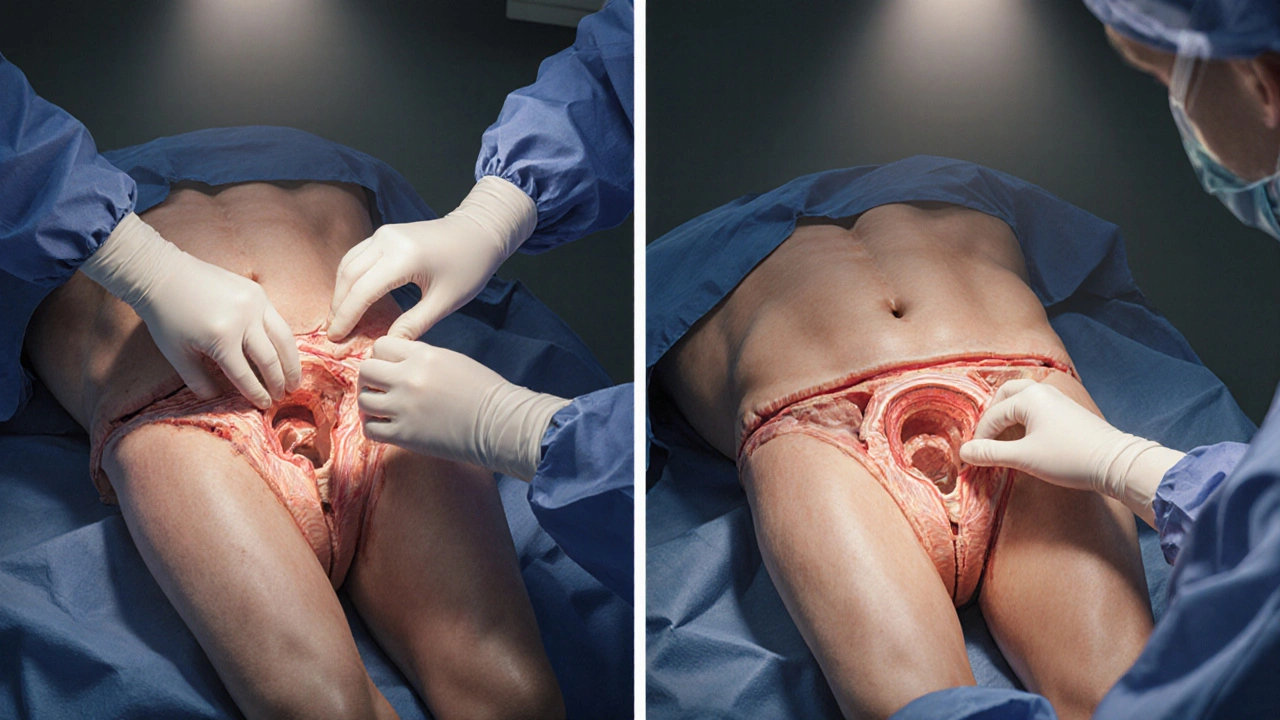
Choosing the Right Surgical Approach
Access to the corpora can be achieved via several routes. Below is a side‑by‑side look at the most common techniques.
| Approach | Incision Site | Typical Indications | Advantages | Potential Drawbacks |
|---|---|---|---|---|
| Scrotal approach | Midline scrotal raphe | Erosion into scrotum, distal cylinder exposure | Direct view of the distal cylinder, short operative time | Limited access to proximal corpora, higher risk of postoperative edema |
| Perineal approach | Mid‑perineum, between the scrotum and anus | Proximal cylinder damage, severe fibrosis | Excellent exposure of proximal corpora, easier removal of adherent cylinders | Deeper dissection, potential for numbness in the perineal skin |
| Combined scrotal‑perineal | Both incisions used sequentially | Complex infections involving the entire prosthesis | Comprehensive debridement, maximises tissue preservation | Longest operative time, higher postoperative discomfort |
Key Steps in a Revision Procedure
- Pre‑op work‑up - Labs (CBC, CRP), ultrasound to assess cylinder location, and culture swabs if infection is suspected.
- Antibiotic protocol - A dose of intra‑operative antibiotic (e.g., cefazolin 2g) is given within 60minutes of incision, followed by a 5‑day oral course tailored to culture results.
- Incision and exposure - The surgeon selects scrotal, perineal, or combined access based on the table above.
- Device removal - Cylinders are gently dissected away from scar tissue. If the implant is fragmented, each piece is retrieved to avoid residual foreign material.
- Debridement - All necrotic tissue is excised, and the corpora are irrigated with a saline‑gentamicin solution.
- Re‑implantation (if immediate) - New cylinders are placed, often of a different size to compensate for any loss of corporal length.
- Closure - Layered closure with absorbable sutures. Drains are rarely needed now; a pressure dressing suffices for most cases.
Post‑operative Care and Outcomes
Recent studies show that a 24‑hour drain‑free protocol reduces infection risk without increasing hematoma rates. The typical recovery plan includes:
- Day0-1: Ice packs, gentle scrotal support, oral analgesics.
- Day2-5: Continue antibiotics, avoid sexual activity, monitor for any discharge.
- Week2: First follow‑up visit; ultrasound checks for fluid collections.
- Week4-6: Gradual re‑introduction of prosthesis activation (if implanted).
Success rates for revision surgery now hover around 85% for infection‑related cases and 90% for mechanical failures, provided the surgeon follows a strict aseptic technique.
Common Pitfalls and How to Avoid Them
- Under‑estimating fibrosis - Skipping a pre‑op ultrasound can lead to surprise during dissection. Always image the corpora.
- Inadequate antibiotics - Empiric coverage without culture data may miss resistant organisms. Tailor therapy.
- Choosing the wrong approach - A scrotal incision for a proximal cylinder fracture forces unnecessary tissue traction. Follow the comparison table.
- Leaving residual parts - Even tiny fragments act as a nidus for infection. Verify complete removal.
When to Seek a Second Opinion
If any of the following apply, it’s wise to consult another urologist experienced in prosthetic surgery:
- Persistent fever or drainage after the first surgery.
- Significant loss of penile length or curvature.
- Repeated mechanical failures within six months.
- Unclear imaging findings about cylinder position.
Future Directions in Prosthesis‑Related Surgery
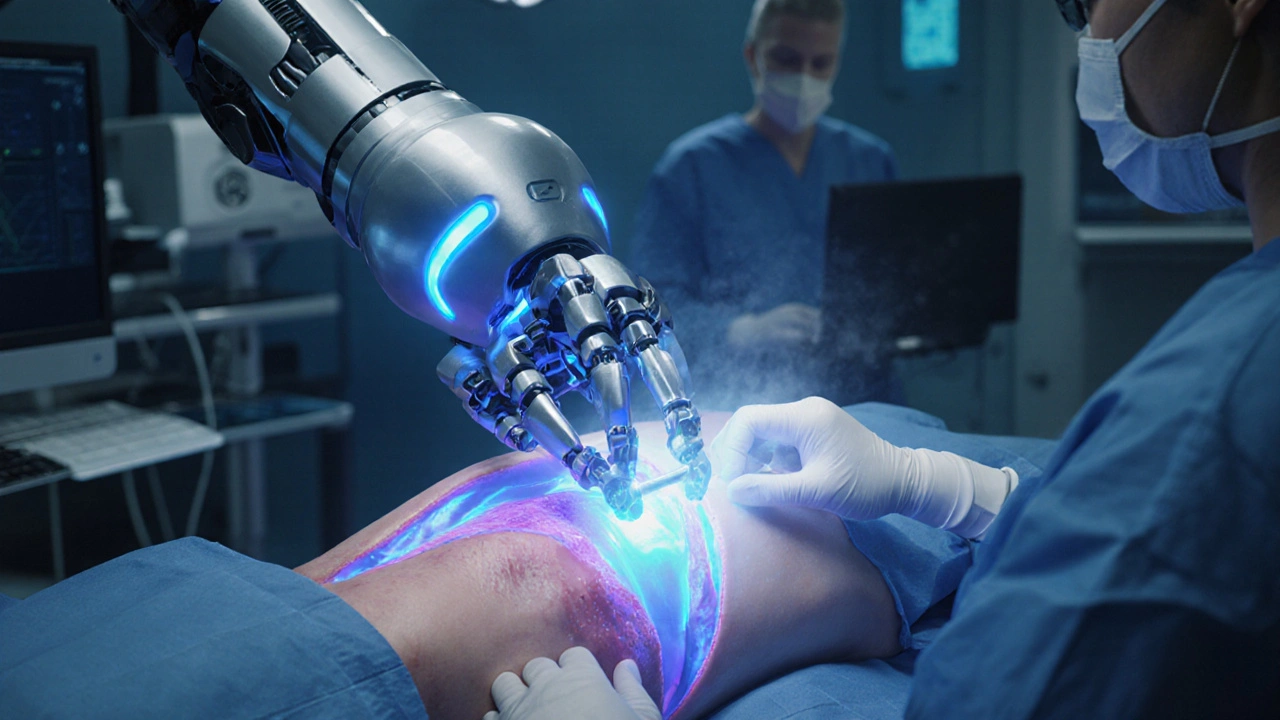
Research in 2024-2025 is focusing on bio‑film resistant coatings and absorbable antibiotic‑laden meshes that could eliminate the need for staged revisions. Meanwhile, robotic assistance for perineal access is being piloted in a few high‑volume centers, promising less tissue trauma and faster recovery.
Frequently Asked Questions
What signs indicate a penile prosthesis infection?
Redness, swelling, warmth, pain, fever, or any drainage from the scrotal incision are classic red flags. If you notice foul‑smelling fluid or pus, contact your surgeon immediately.
Can an infected prosthesis be saved without removal?
Rarely. In early‑stage infections limited to the pocket, aggressive antibiotics and a surgical washout might salvage the device, but most urologists recommend explantation to avoid chronic bio‑film formation.
How long does a staged revision take?
The first surgery clears infection and usually requires 3‑6months of antibiotics and wound healing. The second stage, when a new prosthesis is placed, is a standard implantation procedure lasting 1‑2hours.
Is a perineal incision more painful than a scrotal one?
Pain perception varies, but the perineal route involves deeper tissue layers. Most surgeons provide a longer course of analgesics and recommend a soft cushion to sit on for the first week.
What is the success rate of revision surgery?
Recent multicenter data show an 85‑90% functional success rate when the infection is controlled and the surgeon follows a strict aseptic protocol.