Penile Surgery for Prosthesis Complications: When and How
Explore when and how penile surgery addresses prosthesis complications like infection, erosion, and mechanical failure, with clear steps, approaches, and post‑op care.
When working with penile surgery, any surgical procedure that alters, repairs, or reconstructs the penis. Also known as penile operation, it addresses functional, congenital, or injury‑related issues.
Penile surgery can range from a simple circumcision to a multi‑stage phalloplasty. The core idea is that the penis is a complex organ – it has blood vessels, nerves, erectile tissue, and cosmetic appearance, all of which may need attention. Because of that, surgeons use a toolbox that includes skin grafts, implants, and microsurgical techniques. The goal is always to restore or improve sexual function, urinary flow, or appearance, depending on the patient’s needs.
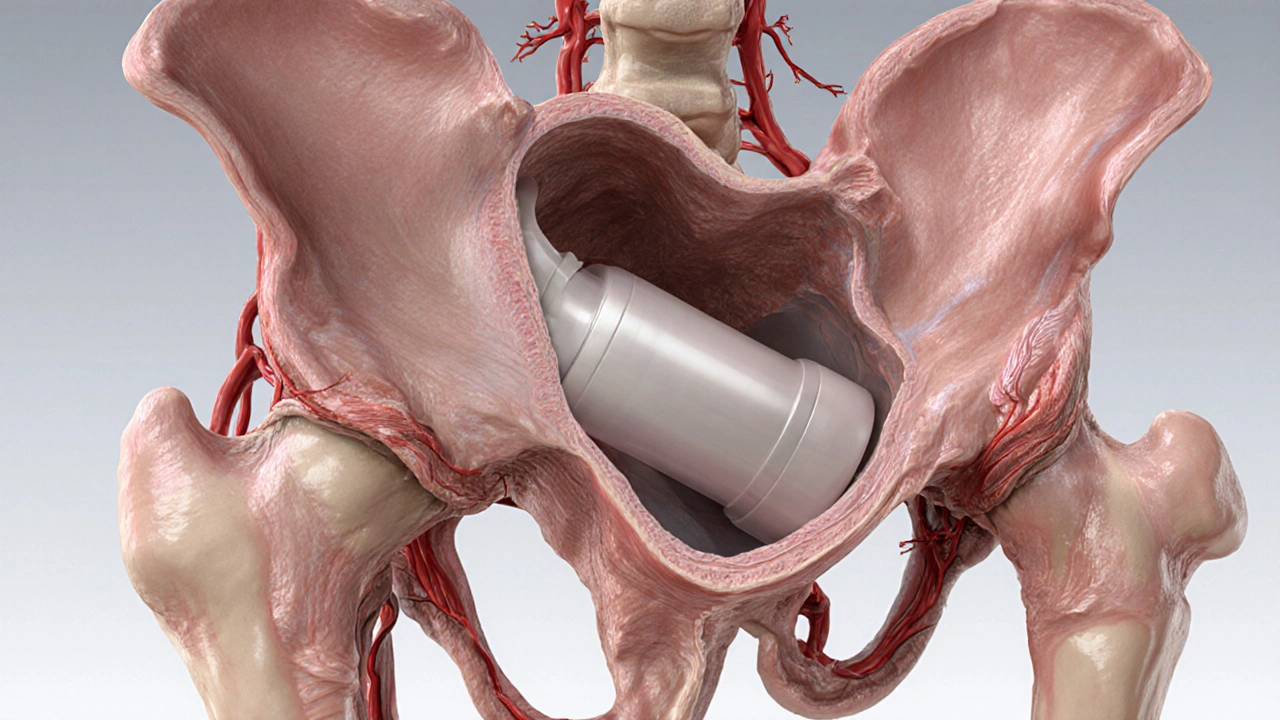
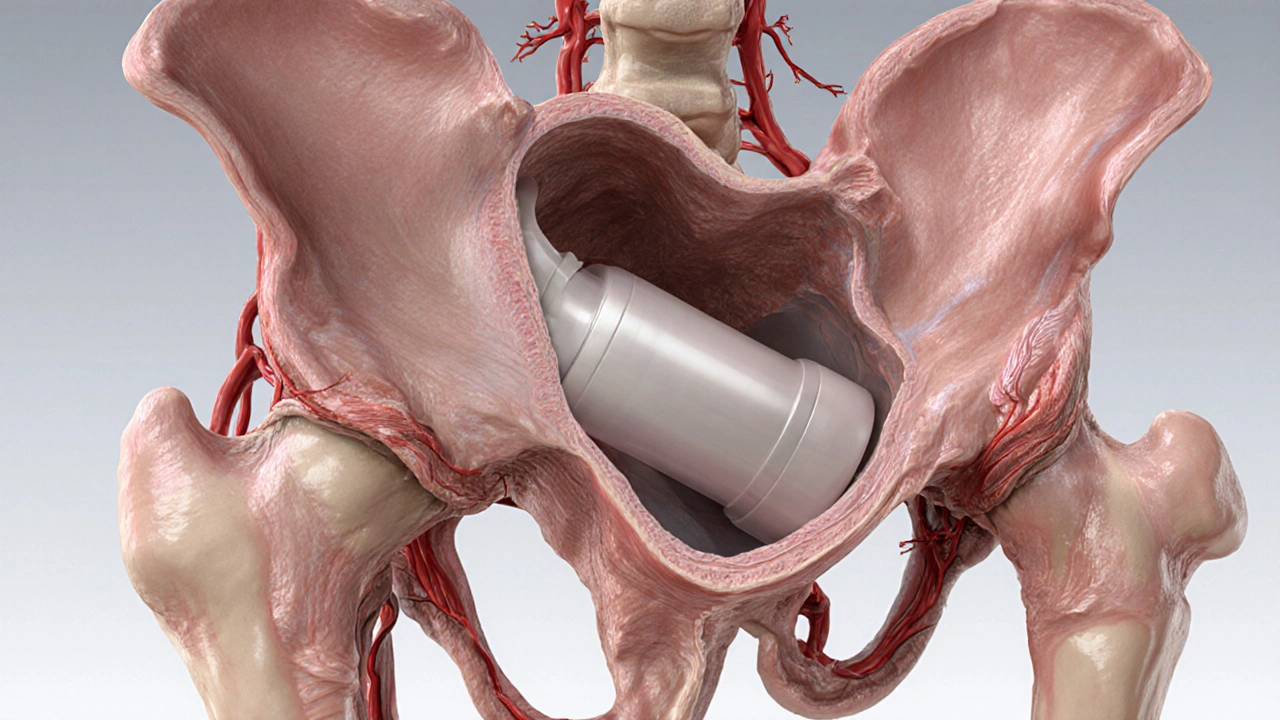
One of the most common reasons patients seek erectile dysfunction, the inability to achieve or maintain an erection suitable for intercourse. Also called ED, this condition often leads to discussions about penile prosthesis, an implanted device that provides rigidity on demand. Physicians known as urologists, medical specialists trained in urinary and male reproductive health guide the decision‑making process. They evaluate whether medication, lifestyle changes, or surgery offers the best chance of success. When a prosthesis is recommended, they explain the types – malleable rods versus inflatable pumps – and match the choice to the patient’s anatomy and lifestyle. This conversation is a key step because the implant’s reliability, sensation, and maintenance requirements differ markedly.
Penile surgery also covers corrective work for congenital conditions such as hypospadias, where the urinary opening is misplaced, and for trauma‑related injuries that affect length or curvature. In gender‑affirming care, phalloplasty is a specialized form of reconstruction that builds a neophallus using tissue flaps. Each of these procedures follows the same principle: a skilled urologist or reconstructive surgeon creates a functional outcome while minimizing complications.
After any procedure, postoperative care, the set of instructions and follow‑up visits that support healing becomes the linchpin of a successful outcome. Patients receive guidance on wound cleaning, activity restrictions, pain management, and signs of infection. Follow‑up appointments let the surgeon check implant positioning, tissue healing, and urinary function. Skipping these steps can lead to scar tissue, prosthesis malfunction, or persistent pain. Good postoperative care influences healing outcomes and reduces the chance of revision surgery.
Understanding these connections – how erectile dysfunction can lead to a prosthesis, how urologists perform the operation, and how postoperative care shapes recovery – helps you weigh your options. Below you’ll find detailed guides on each topic, from choosing the right implant to managing daily care after surgery, so you can move forward with confidence.
Explore when and how penile surgery addresses prosthesis complications like infection, erosion, and mechanical failure, with clear steps, approaches, and post‑op care.