For decades, Medicare wasn’t allowed to negotiate drug prices. That changed in 2022 with the Inflation Reduction Act. Starting January 1, 2026, Medicare will directly bargain with drug companies over the cost of 10 high-priced medications - and the discounts are massive. Some drugs are now priced 79% lower than before. This isn’t a small tweak. It’s a full overhaul of how billions in drug spending get handled in the U.S.
What drugs are affected?
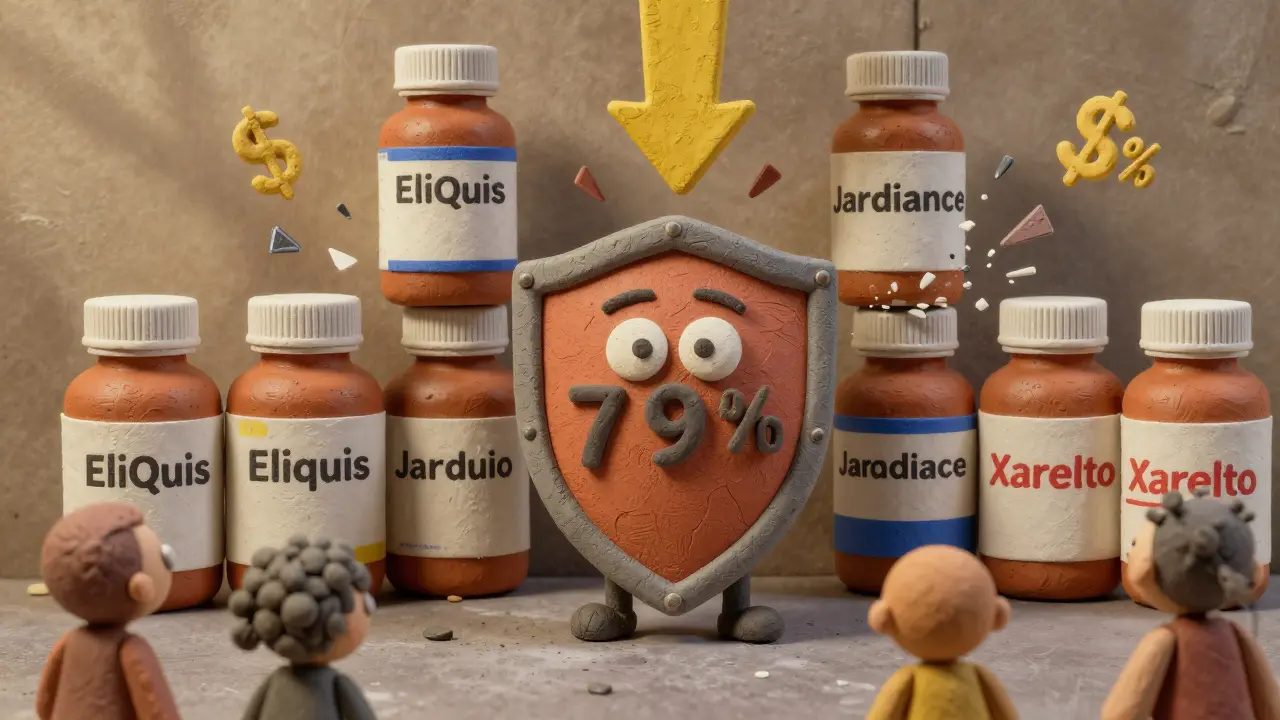
The first 10 drugs chosen for negotiation aren’t obscure generics. These are blockbuster medications millions of Americans rely on every day. Eliquis (for blood clots), Jardiance (for diabetes), Xarelto (another blood thinner), and others like Farxiga and Stelara are all on the list. These drugs made over $50 billion in Medicare spending in 2022 alone. Eliquis, for example, cost Medicare $6.3 billion in one year. Before the law, drugmakers set prices with zero government oversight. Now, Medicare has the power to say, "This is what we’re paying."How does the negotiation actually work?
It’s not a backroom deal. The process is written into law with clear steps. On February 1, 2024, Medicare sent each drug company its first offer - backed by data on what similar drugs cost, how often the drug is used, and what alternatives exist. The companies had 30 days to respond. Then came three official negotiation meetings between March and August 2024. Five of the 10 drugs reached agreements during those talks. The other five were settled through final written offers.Medicare’s offer wasn’t random. It was based on two strict limits. First, it couldn’t go higher than the average price Medicare Part D plans actually paid after rebates and discounts. Second, it couldn’t exceed a percentage of the drug’s average price across all U.S. markets (called non-FAMP). This stopped companies from claiming their drug was "special" and worth way more than others.
The result? Discounts ranged from 38% to 79%. For Eliquis, the price dropped by 67%. For Jardiance, it was 75%. That means a 30-day supply that used to cost $500 might now cost $125. These new prices take effect on January 1, 2026 - and they’ll apply to every Medicare Part D plan in the country.
Why this matters for patients
If you’re on Medicare and take one of these drugs, your out-of-pocket costs will drop. Right now, many seniors pay hundreds of dollars a month. With the new prices, some will pay less than $20 per month. That’s huge for people on fixed incomes. The savings aren’t just for those in the "donut hole" - they ripple through all coverage phases. Even people in catastrophic coverage will benefit because the plan’s overall costs go down, which can reduce premiums over time.But here’s the catch: not every drug will be affected. Only drugs that are at least 7 years old (or 11 for biologics) and have no generic or biosimilar competition are eligible. That means newer drugs - like those approved in the last few years - won’t be touched yet. But starting in 2027, 15 more drugs will join the list. By 2028, the program expands to Part B drugs - the ones given in doctors’ offices, like cancer treatments. That’s when more people will feel the impact.

What about private insurance?
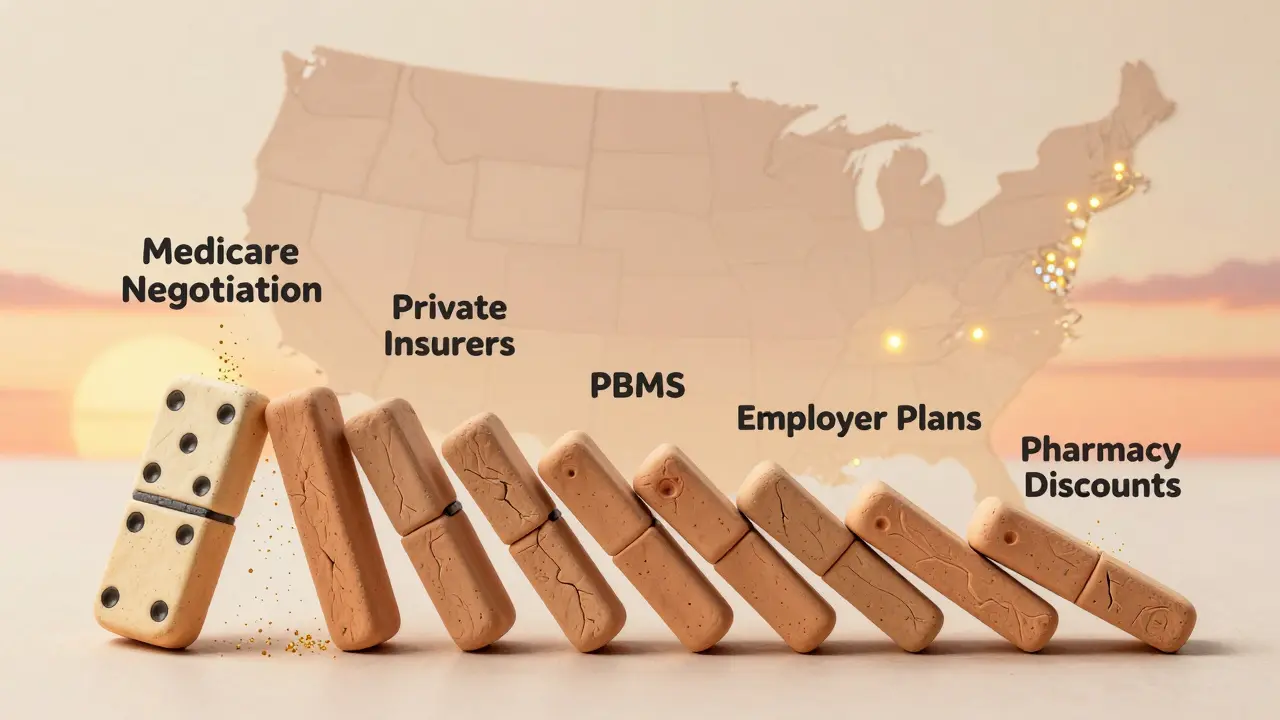
You might think this only affects Medicare. But it doesn’t stop there. Private insurers are watching closely. When Medicare cuts a price, manufacturers often lower the price for everyone else - not because they have to, but because they don’t want to deal with multiple pricing tiers. This is called the "spillover effect." Experts estimate private insurers could save $200-250 billion over the next decade just because Medicare set a new benchmark.Pharmacy benefit managers (PBMs) and employers are already adjusting their contracts. Some are now demanding similar discounts for drugs not yet on Medicare’s list. It’s like a domino effect. One change in government pricing ripples through the entire system.
What’s the backlash?
Drug companies didn’t go quietly. Four of the 10 manufacturers sued, claiming the law is unconstitutional. A federal judge dismissed those lawsuits in August 2024, but appeals are expected. The pharmaceutical industry argues this will hurt innovation. They say if companies can’t charge high prices, they won’t invest in new drugs. But the Office of Management and Budget found those claims were exaggerated - by as much as 50%.Doctors are also adjusting. For Part B drugs, reimbursement will shift from "average sales price plus 6%" to "negotiated price plus 6%." That means clinics may earn less for giving out certain injections. Some practices are already planning how to handle the drop in revenue. The American Medical Association warns this could lead to fewer providers offering certain treatments - especially in rural areas.
What’s next?
The program is just getting started. The second round of 15 drugs for 2027 was announced in January 2024. That list includes drugs like Farxiga and Stelara. By 2028, Medicare will start negotiating prices for Part B drugs - the ones you get in a clinic or hospital. That’s where the real money is: cancer drugs, rheumatoid arthritis treatments, and other high-cost infusions.There’s talk about making the rules even stronger. Some lawmakers want to reduce the eligibility age from 7 years to 5 years. If that happens, dozens more drugs could qualify for negotiation every year. The FTC is also cracking down on tactics drugmakers use to delay generics - like making tiny changes to a drug just to reset the clock on exclusivity. These moves are slowly closing loopholes.
What this means for you
If you’re on Medicare and take a high-cost drug, expect your bills to drop in 2026. You won’t need to do anything. Your plan will update automatically. But if you’re not on Medicare, don’t assume you’re unaffected. Your employer’s insurance, your private plan, or even your pharmacy’s discount program may start offering lower prices too.This isn’t about politics. It’s about fairness. For years, the U.S. paid more for the same drugs than any other developed country. Canada, the UK, and Germany have long used negotiation to keep prices in check. Now, Medicare is catching up. The savings aren’t theoretical. They’re real. And they’re starting now.
Will my Medicare Part D premiums go down because of these price cuts?
Not immediately, but likely over time. Premiums are set annually based on the total cost of drugs covered by the plan. When Medicare negotiates lower prices, the overall cost of the drug benefit drops. That gives plans room to lower premiums in future years. You won’t see a cut in 2026, but by 2027 or 2028, many plans may reduce monthly costs.
Can I still get my brand-name drug if it’s negotiated?
Yes. The negotiation lowers the price - it doesn’t remove the drug from your plan. Your doctor can still prescribe Eliquis, Jardiance, or any other negotiated drug. The only change is that Medicare will pay less for it, and your out-of-pocket cost will likely drop too.
Why are only 10 drugs being negotiated in 2026?
The law was designed to start small. The first year focused on the 10 drugs with the highest Medicare spending and no competition. This lets the system test the process before expanding. Starting in 2027, 15 drugs will be added. By 2029, up to 20 drugs per year will be negotiated - enough to cover the majority of high-cost, single-source drugs.
Do these price cuts apply to people under 65 on Medicare?
Yes. Anyone enrolled in Medicare Part D - whether you’re 65 or younger due to disability or end-stage renal disease - will benefit. The negotiated prices apply to all Part D enrollees, no matter the reason for eligibility.
What if my drug isn’t on the list yet?
It may be soon. The list expands every year. If your drug is at least 7 years old (or 11 for biologics) and has no generic or biosimilar version, it could be selected in the next cycle. Keep an eye on CMS’s annual announcements - they’re published every January. You can also check the official Medicare website for updates.