Eye Infection Symptom Checker
This tool helps differentiate between bacterial eye infections and conjunctivitis by analyzing symptoms.
Quick Take
- Bacterial eye infections are caused by specific germs like Staphylococcus aureus and need antibiotics.
- Conjunctivitis is an inflammation of the conjunctiva and can be bacterial, viral, or allergic.
- Symptoms overlap-redness, discharge, irritation-but bacterial cases often produce thicker, yellow‑green pus.
- Diagnosis usually involves a quick eye exam; swabs are taken only for severe or atypical cases.
- Good hygiene, proper contact‑lens care, and timely treatment keep most infections from spreading.
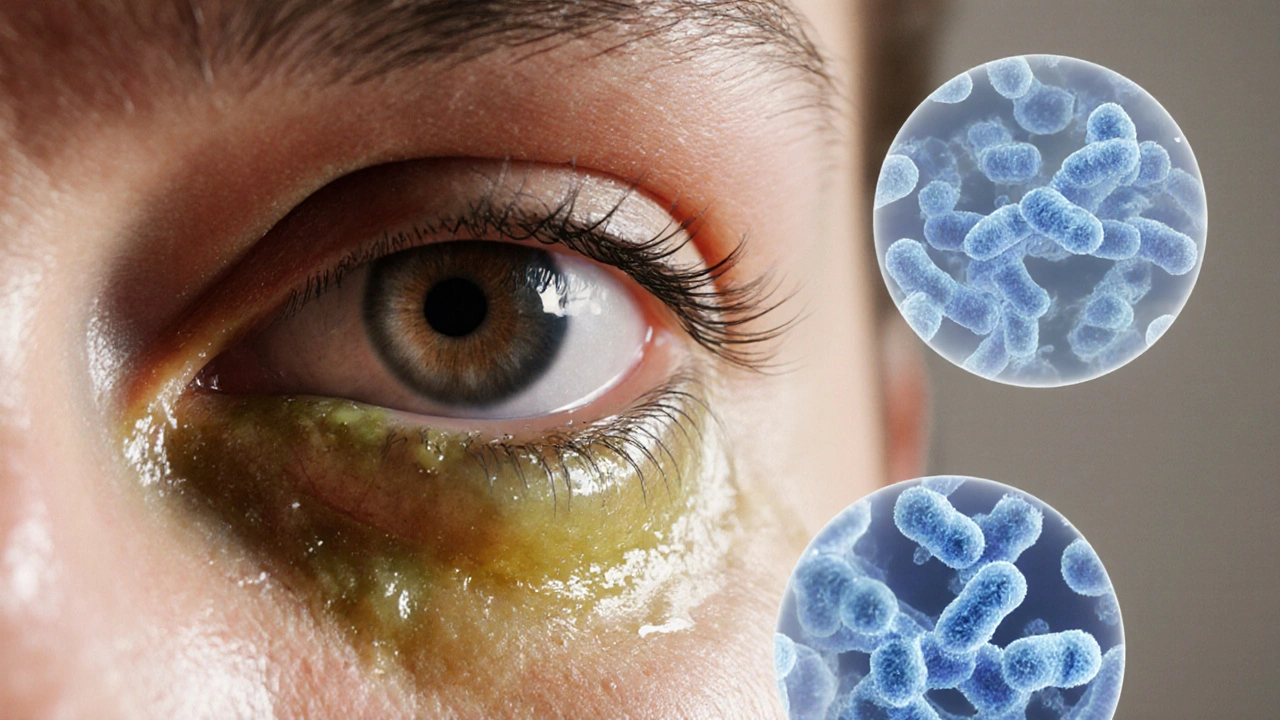
What Is a Bacterial Eye Infection?
When a bacterial eye infection occurs, harmful bacteria invade the ocular surface, causing inflammation, pain, and a variety of discharge types, the eye becomes red and uncomfortable. Common forms include blepharitis (eyelid margin infection), keratitis (corneal infection), and dacryocystitis (tear‑duct infection). While any bacterial species can theoretically cause trouble, a handful show up far more often.
Understanding Conjunctivitis
Conjunctivitis is the inflammation of the thin, transparent membrane (conjunctiva) that lines the eyelid and covers the white part of the eye. It’s not a single disease but a symptom complex that can stem from bacteria, viruses, allergies, or irritants. The term "pink eye" usually points to the viral variety, yet many people conflate any redness with bacterial infection.
Common Bacterial Culprits
- Staphylococcus aureus Gram‑positive cocci that frequently colonize the skin and eyelids, leading to blepharitis and corneal ulcers
- Streptococcus pneumoniae A common cause of conjunctivitis and keratitis, especially after eye injury
- Haemophilus influenzae Often implicated in pediatric bacterial conjunctivitis and can spread quickly in daycare settings
- Moraxella catarrhalis Usually found in the upper respiratory tract; can cause chronic conjunctivitis in adults
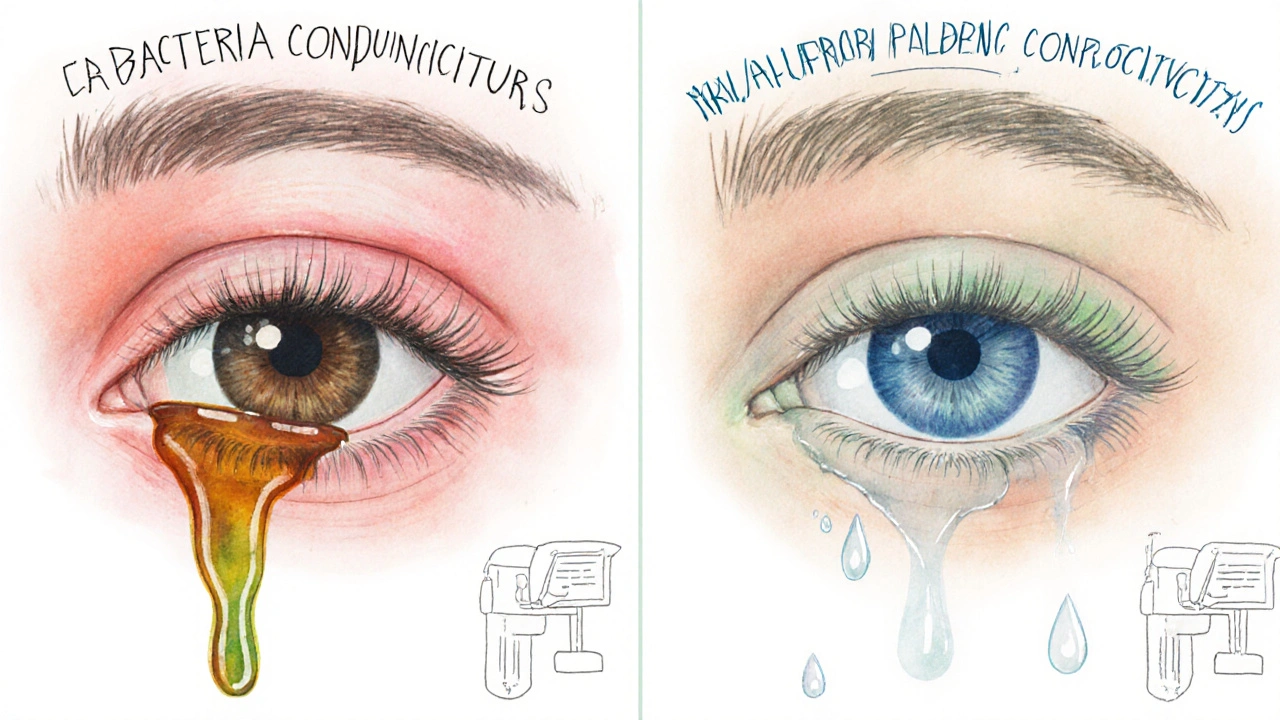
Symptoms: How to Spot the Difference
Both conditions share a red eye, itching, and a feeling of grit. The devil’s in the details:
- Bacterial eye infection: Thick, yellow‑green or brownish discharge that may crust over the lashes overnight. Pain tends to be more pronounced, especially with keratitis.
- Conjunctivitis (viral): Watery or mucoid discharge, often starting in one eye and quickly moving to the other. Itching is common, and fever may accompany a viral illness.
- Conjunctivitis (allergic): Intense itching, stringy clear discharge, and often a history of seasonal allergies or exposure to irritants.
If you notice a sudden loss of vision, intense light sensitivity, or a hard, raised spot on the cornea, seek care immediately-those signs point to a more serious bacterial invasion.
Diagnosis: Tests and When to See a Doctor
Most eye doctors can differentiate the cause based on visual inspection. For routine cases, a slit‑lamp exam reveals the location and character of the inflammation.
When the presentation is atypical, the clinician may take a conjunctival swab. The specimen is cultured on chocolate agar or blood agar to identify the exact bacterium, a step that guides targeted antibiotic therapy.
Treatment Options
Because bacteria are living organisms, they respond to antimicrobial agents. The first‑line approach for uncomplicated bacterial conjunctivitis is topical antibiotic eye drops such as moxifloxacin, tobramycin, or azithromycin, applied four to six times daily for 5‑7 days. If the infection involves the cornea (keratitis) or deep structures, oral antibiotics like doxycycline may be added.
Viral and allergic forms do not benefit from antibiotics; instead, they are managed with supportive care-artificial tears, antihistamine drops, or cold compresses.
Never share eye drops, and always discard them after the prescribed course-resistance can develop if treatment is stopped early.
Prevention Tips
- Wash your hands frequently with soap, especially before touching your eyes.
- Disinfect contact lenses and storage cases daily; replace lenses as recommended.
- Avoid swimming with contacts or in overly chlorinated pools.
- Don’t rub your eyes; use a clean tissue if you need to wipe away discharge.
- Replace eye makeup every three months and avoid sharing mascara or eyeliner.
Side‑by‑Side Comparison
| Aspect | Bacterial Eye Infection | Conjunctivitis (Viral/Allergic) |
|---|---|---|
| Typical Causes | Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae | adenovirus, rhinovirus, pollen, pet dander |
| Discharge | Thick, yellow‑green, may crust | Watery or clear, stringy (allergic) |
| Pain Level | Moderate to severe, especially with keratitis | Mild itching, burning |
| Contagiousness | Can spread via hands or shared items | Highly contagious (viral); not contagious (allergic) |
| Treatment | Antibiotic eye drops or oral antibiotics | Supportive care, antihistamines, antiviral meds rarely needed |
| Recovery Time | 5‑7 days with proper antibiotics | 7‑14 days for viral; varies for allergic |
When to Seek Emergency Care
Even though most bacterial eye infections are treatable, certain warning signs demand urgent attention:
- Sudden vision loss or blurriness
- Severe eye pain that doesn’t improve with OTC lubricants
- Visible white or grey spot on the cornea
- High fever accompanying eye symptoms
- Swelling that spreads to the eyelids or surrounding skin
Prompt evaluation can prevent permanent scarring or loss of sight.
Frequently Asked Questions
Can viral conjunctivitis turn into a bacterial infection?
Yes. If the eye’s protective barrier is compromised-by rubbing or secondary bacterial colonization-a viral case can become mixed with bacteria, which then requires antibiotics.
Are over‑the‑counter eye drops effective for bacterial infections?
OTC artificial tears or antihistamine drops can soothe symptoms but won’t eradicate bacteria. Prescription antibiotic drops are necessary for a true bacterial eye infection.
How long are antibiotics needed for eye infections?
Typically 5‑7 days of topical drops. For deeper infections like keratitis, a longer course-often 10‑14 days-may be prescribed, sometimes combined with oral therapy.
Can contact lens wearers get bacterial eye infections?
Absolutely. Improper cleaning, overnight wear, or using expired solution creates a perfect breeding ground for bacteria like Staphylococcus aureus.
Is it safe to use leftover antibiotics for another eye infection?
No. Different bacteria may require different agents, and using an incomplete course can fuel resistance. Always let a clinician prescribe a fresh regimen.