Amitriptyline Overdose Symptom Checker
Assess your symptoms
Select any symptoms you're experiencing. This tool is not a diagnosis but can help you recognize urgent situations.
When someone takes too much amitriptyline overdose, every minute counts. Knowing the red‑flag signs, the life‑threatening symptoms, and the right steps to get help can be the difference between a full recovery and permanent damage.
What is Amitriptyline?
Amitriptyline is a tricyclic antidepressant (TCA) prescribed for depression, neuropathic pain, and migraine prevention. It works by boosting the levels of serotonin and norepinephrine in the brain, while also blocking certain receptors that affect heart rhythm and muscle tone. Because it touches many body systems, taking more than the therapeutic dose can spark a cascade of dangerous reactions.
How does an overdose happen?
Most accidental overdoses occur when a patient forgets the exact dose, mixes the drug with alcohol, or tries to self‑medicate for severe pain. Intentional overdoses, unfortunately, are a common method in suicide attempts. The toxic threshold varies with age, weight, and liver function, but‑for adults‑serious effects often appear after 300mg taken at once, and lethal outcomes have been reported above 750mg.
Early warning signs (mild to moderate)
In the first hour, the body reacts with what clinicians call anticholinergic effects. Look for:
- Dry mouth and metallic taste
- Blurred vision or dilated pupils
- Flushed skin and heat intolerance
- Constipation or urinary retention
- Rapid, shallow breathing (tachypnea)
These symptoms can mimic a bad cold, so they’re easy to dismiss-but they signal that the drug is already overloading the nervous system.
Severe symptoms (life‑threatening)
When the dose climbs into the high‑toxicity zone, the drug’s impact on the heart and brain takes over. Watch for:
| Category | Signs | Potential Outcome |
|---|---|---|
| Cardiac | Prolonged QT interval, widened QRS complex | Arrhythmias, cardiac arrest |
| Neurological | Seizures, confusion, coma | Permanent brain injury |
| Respiratory | Apnea, severe hypoxia | Organ failure |
| Metabolic | Acidosis (blood pH < 7.35) | Multi‑system collapse |
These patterns are driven by two core toxic mechanisms. First, the anticholinergic effect shuts down parasympathetic control, leading to dry secretions and slowed gut motility. Second, the drug’s cardiac toxicity blocks sodium channels in heart muscle, widening the QRS complex and predisposing the heart to ventricular arrhythmias.
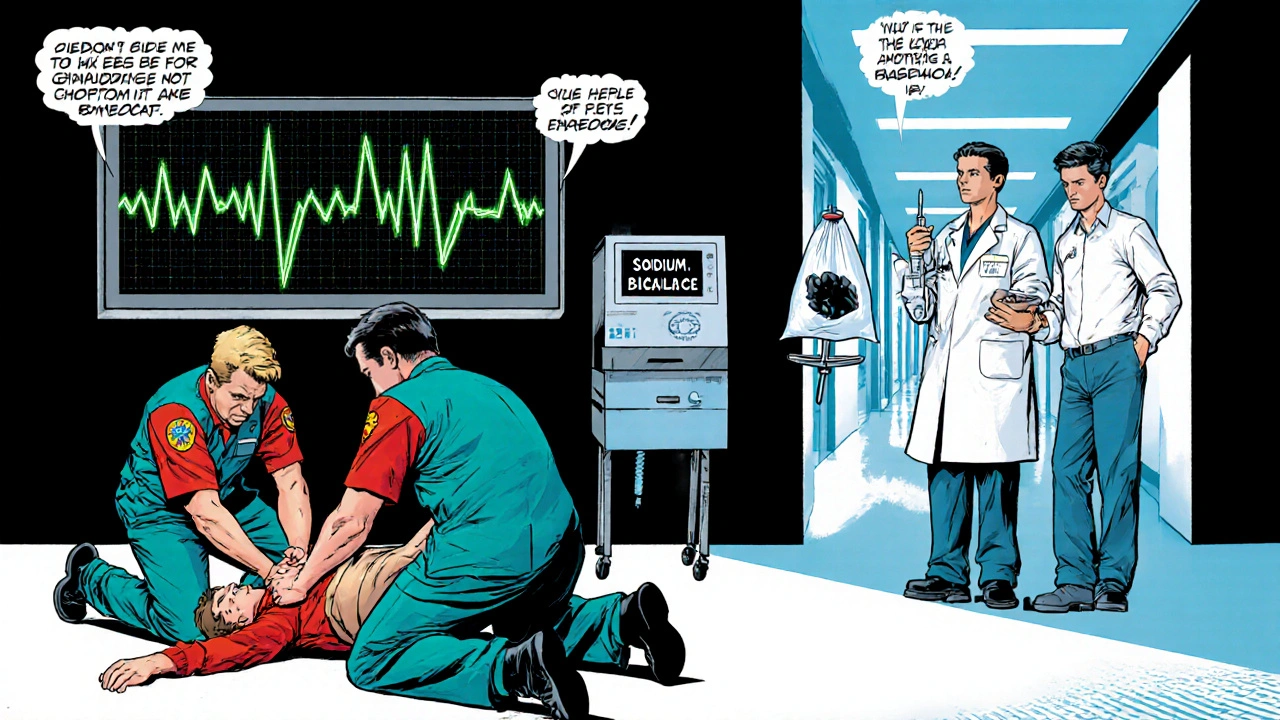
What to do immediately (first aid)
- Call emergency services (999 in the UK) right away. Mention "suspected Amitriptyline overdose" so the paramedics can prep the right equipment.
- If the person is conscious and able to swallow, give them a glass of water. Do NOT induce vomiting unless a medical professional tells you to.
- Check breathing and pulse. If breathing stops, start CPR and continue until help arrives.
- Gather any pill bottles, prescription records, or empty blister packs. This information helps the toxicology team determine the exact dose.
Time is critical because the drug is rapidly absorbed from the gut. Within 30‑60minutes, blood levels peak, and the heart may already be in trouble.

Medical treatment options
In the hospital, doctors follow a clear protocol.
- Activated charcoal is given orally or via a nasogastric tube within the first hour. It binds the drug in the gut, preventing further absorption.
- If cardiac toxicity is evident (QRS > 100ms), sodium bicarbonate is infused. The alkaline solution narrows the QRS complex by reducing the drug’s binding to sodium channels.
- Seizures are treated with benzodiazepines (e.g., lorazepam). Traditional antiepileptic drugs like phenytoin are avoided because they can worsen cardiac conduction.
- Intensive monitoring includes continuous ECG, arterial blood gases, and serum amitriptyline levels when available.
In extreme cases, extracorporeal membrane oxygenation (ECMO) or repeated doses of sodium bicarbonate may be required to keep the heart beating.
Prevention tips
Even though accidents happen, many overdoses are preventable.
- Store all medication out of reach of children and visitors.
- Use a pill organizer and set daily alarms to avoid double‑dosing.
- Never mix Amitriptyline with alcohol or other sedatives; the combined depressant effect can tip the balance quickly.
- If you feel your dose isn’t controlling pain, talk to your GP before adjusting it yourself.
- Dispose of unused tablets at a pharmacy take‑back program; don’t keep them in a drawer.
For patients with a history of depression or suicidal thoughts, discuss a safety plan with a mental‑health professional and keep emergency contact numbers handy.
Frequently Asked Questions
What is the lethal dose of Amitriptyline?
Lethal outcomes have been reported after ingesting 750mg or more in adults, though severe toxicity can start at 300mg. Individual factors such as age, weight, and liver function dramatically shift the threshold.
Can activated charcoal reverse an Amitriptyline overdose?
Activated charcoal can bind up to 30‑40% of the drug if given within the first hour, reducing further absorption. It does not reverse toxicity already in the bloodstream, so it works best as an early intervention.
Why is sodium bicarbonate used for heart problems caused by the overdose?
Sodium bicarbonate alkalinizes the blood, which decreases Amitriptyline’s affinity for cardiac sodium channels. This narrows the widened QRS complex and lowers the risk of fatal arrhythmias.
Should I try to make the person vomit?
No. Inducing vomiting can cause aspiration, especially since Amitriptyline depresses the gag reflex. Let medical professionals handle gastric decontamination.
What long‑term effects can result from a severe overdose?
Survivors of severe toxicity may face persistent cardiac conduction abnormalities, memory deficits from hypoxic brain injury, or chronic anxiety about medication use. Follow‑up with cardiology and neurology is often recommended.

