Warfarin Side Effects: What You Need to Know Before Taking It
When you take warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, artificial heart valves, or deep vein thrombosis. Also known as Coumadin, it saves lives by stopping dangerous clots—but it doesn’t come without risks. The biggest concern? Warfarin side effects that can turn minor cuts into serious bleeding events. Unlike newer anticoagulants, warfarin doesn’t have a fixed dose. Your body’s response changes based on diet, other meds, even your genes. That’s why regular blood tests (INR) are non-negotiable.
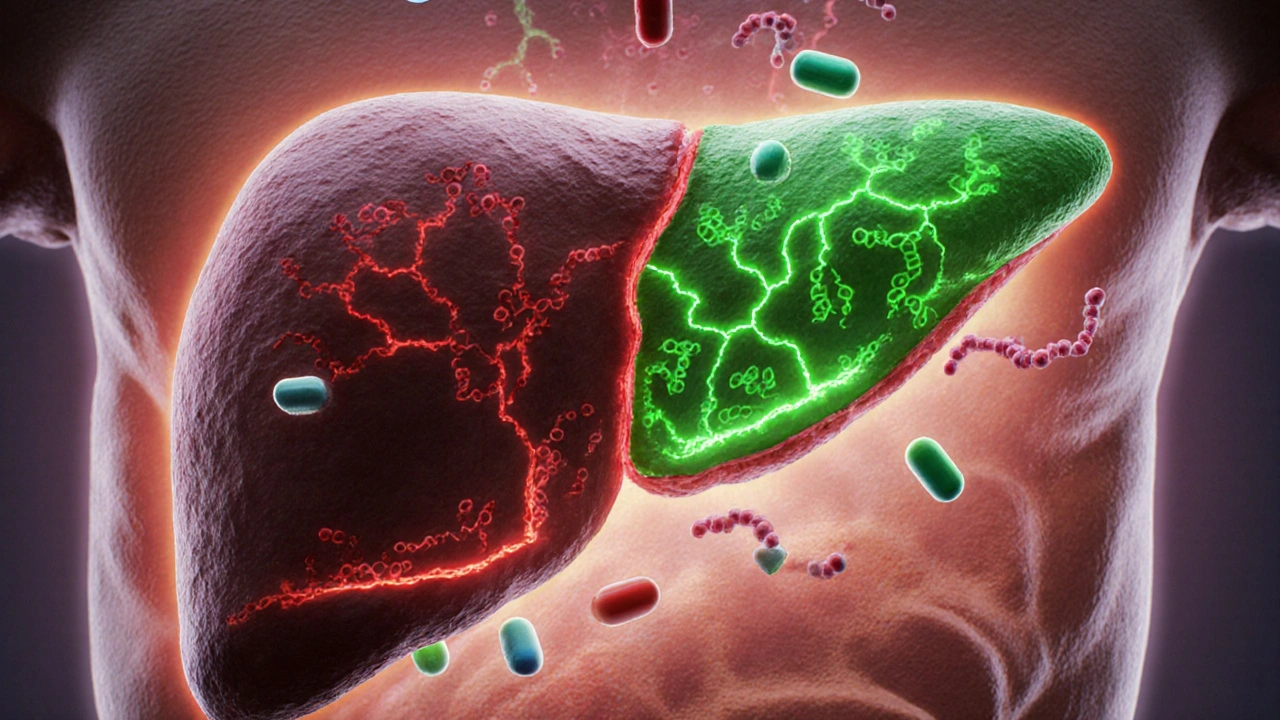
Warfarin works by blocking vitamin K, which your liver needs to make clotting factors. But vitamin K is everywhere—in leafy greens, broccoli, even some supplements. Eat more kale one week and your INR might drop. Skip greens and your blood gets too thin. That’s why consistency matters more than perfection. You don’t need to avoid these foods, just keep your intake steady. Other common drug interactions, happen when antibiotics, painkillers, or even herbal products like St. John’s wort interfere with how warfarin is processed. Some antibiotics can spike your INR overnight. Ibuprofen? It raises your risk of stomach bleeds. Even a single dose of aspirin can be dangerous if you’re on warfarin.
Then there’s the silent danger: INR levels, a blood test that measures how long it takes your blood to clot, with a target range usually between 2.0 and 3.0 for most patients. If your INR is too low, clots form. Too high, and you risk internal bleeding—brain, gut, even your muscles. Symptoms aren’t always obvious. A headache that won’t quit? A swollen, painful leg? Unexplained bruising? A nosebleed that won’t stop? These aren’t normal. They’re red flags. Many people don’t realize they’re bleeding internally until it’s too late. That’s why knowing your numbers and reporting changes fast is critical.
Warfarin isn’t a drug you take and forget. It demands attention. You need to track what you eat, what you take, and when you get tested. Some people handle it fine for years. Others struggle with constant dose changes. It’s not for everyone—but for many, it’s the best option. The posts below cover real cases: how warfarin interacts with common meds, what to do when INR goes wild, how diet affects clotting, and what alternatives exist when warfarin becomes too risky. You’ll find practical advice from people who’ve lived through it—not just textbook warnings. This isn’t about fear. It’s about control.