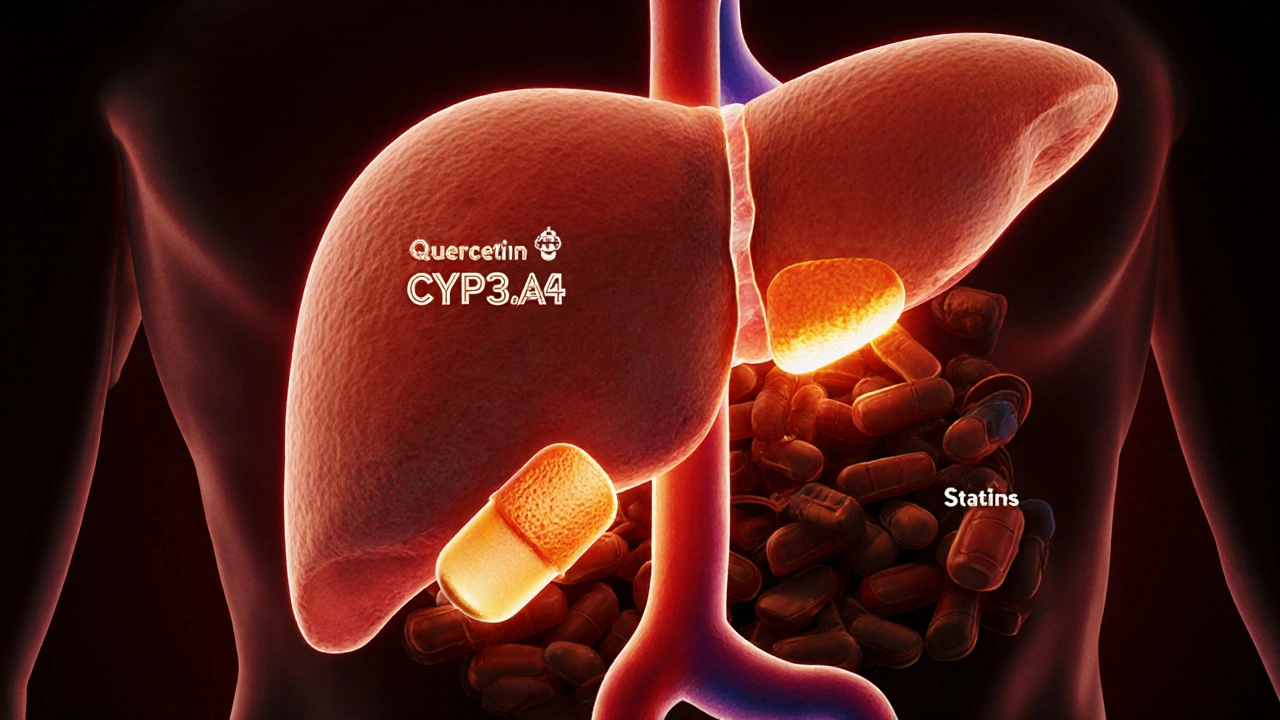
Quercetin and Medications: How Supplement Use Can Alter Drug Levels
Quercetin supplements can block liver enzymes that break down medications, leading to dangerous drug buildup. Learn which meds are at risk and how to stay safe.
When you take a supplement-drug interaction, a chemical conflict between a dietary supplement and a prescription or over-the-counter medication that alters how either works in your body. Also known as herbal-medication interaction, it can turn a safe routine into a health risk—sometimes without warning. Many people assume that because supplements are "natural," they’re harmless. But that’s not true. A daily fish oil pill might thin your blood too much when you’re also on warfarin. A magnesium supplement could block your antibiotic from working. Even something as simple as grapefruit juice can make your cholesterol drug dangerously strong.
These interactions aren’t rare. They happen every day, often because people don’t tell their doctor they’re taking dietary supplements, products taken orally to add nutrients or other substances to the diet, including vitamins, minerals, herbs, and amino acids. Or they assume their pharmacist knows everything on their shelf. But most pharmacists don’t track every supplement you buy online or at a gas station. And many supplements don’t even list their full ingredients. The prescription drugs, medications approved by health authorities for treating specific conditions, often with strict dosing and monitoring requirements. you take—like lithium, antidepressants, blood thinners, or heart meds—can react in ways you never expect. Lithium levels can spike if you start taking a new diuretic or herbal tea. SSRIs can trigger serotonin syndrome when mixed with St. John’s wort. These aren’t hypotheticals—they’re documented in real cases, and they land people in the ER.
herbal remedies, plant-based products used for medicinal purposes, often marketed as natural alternatives to pharmaceuticals. are especially tricky. People think they’re safe because they’ve been used for centuries. But centuries of use doesn’t mean they’re safe with modern drugs. Kava can damage your liver when combined with acetaminophen. Garlic supplements can increase bleeding risk during surgery. Echinacea might interfere with immune-suppressing drugs after a transplant. The problem isn’t just the supplement itself—it’s that most people don’t know what’s in it, how much is active, or how it behaves in the body. Unlike drugs, supplements aren’t required to prove safety or consistency before hitting the market.
You don’t need to quit all supplements. But you do need to be smarter. Know what you’re taking. Write it down. Show it to your doctor or pharmacist every time you get a new prescription. Don’t assume your multivitamin is harmless. Don’t trust a label that says "pure" or "natural." The real question isn’t whether something is natural—it’s whether it’s safe with what you’re already taking. The posts below break down real cases: how protein affects Parkinson’s meds, why some generics change your lithium levels, how proton pump inhibitors clash with heart drugs, and what happens when you take meds with food. These aren’t theory—they’re lived experiences. And they’re the kind of details that keep you out of the hospital.
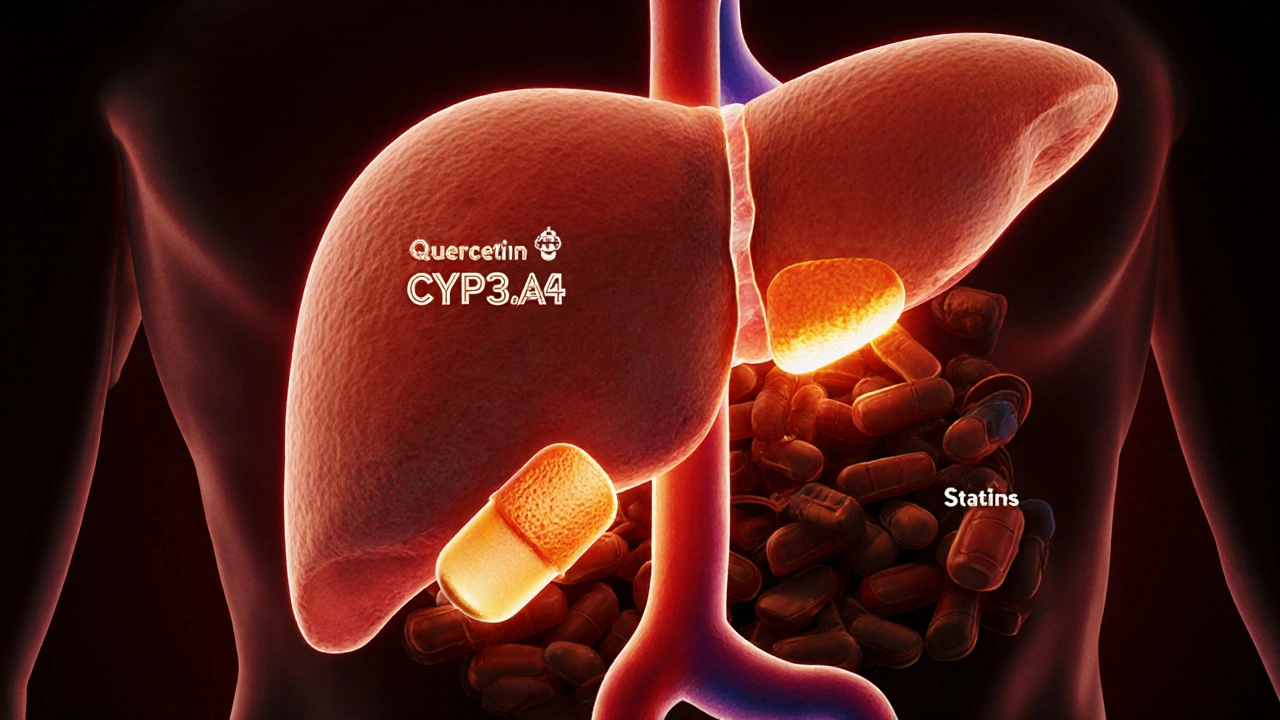
Quercetin supplements can block liver enzymes that break down medications, leading to dangerous drug buildup. Learn which meds are at risk and how to stay safe.