Immunosuppressants: What They Are, How They Work, and Which Medications Are Used
When your immune system turns against your own body, it can cause serious damage. That’s where immunosuppressants, drugs that reduce the activity of the immune system to prevent damage from overreaction. Also known as anti-rejection drugs, they are essential for people who’ve had organ transplants and those with autoimmune conditions like rheumatoid arthritis or Crohn’s disease. These aren’t antibiotics or painkillers—they don’t kill germs or ease discomfort. Instead, they quietly dial down the immune system’s attack mode, stopping it from destroying healthy tissue or rejecting a new kidney, liver, or heart.
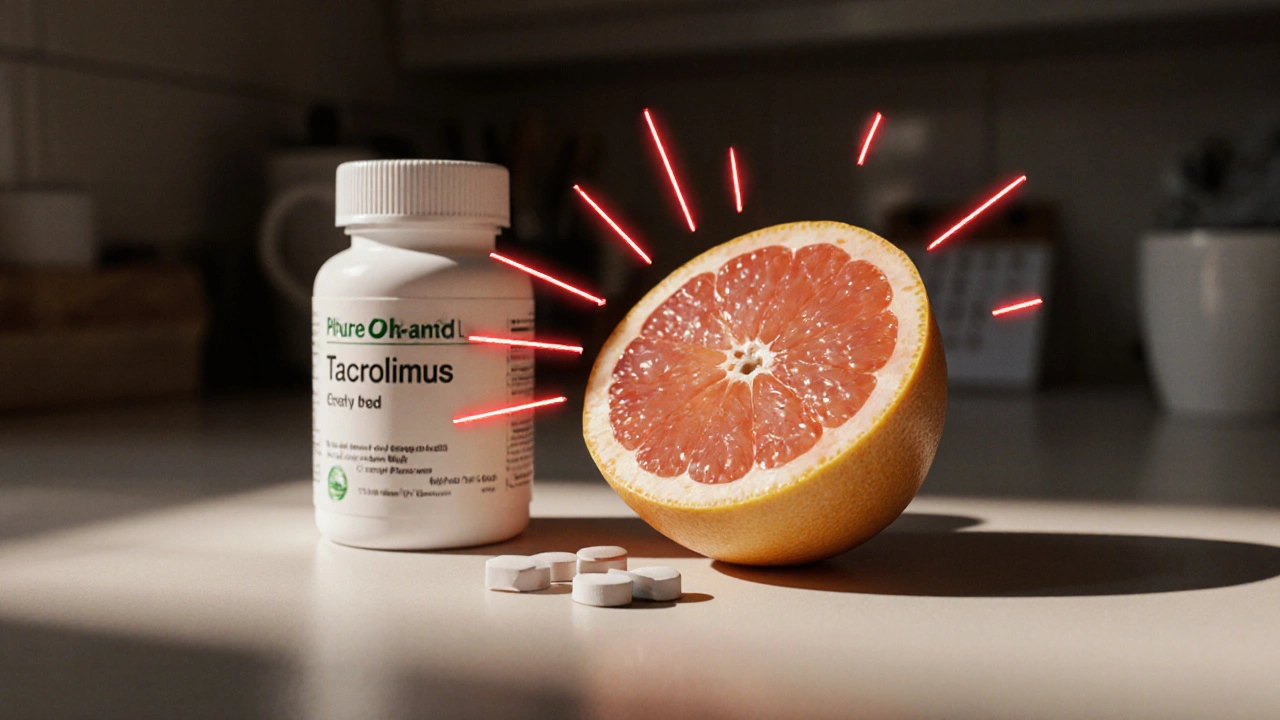
Immunosuppressants come in different types, each with a different target. corticosteroids, like prednisone, reduce inflammation and suppress broad immune activity—they’re often used short-term because of side effects like weight gain and bone loss. Then there are biologic drugs, targeted therapies that block specific immune proteins like TNF-alpha, used for conditions like ankylosing spondylitis or psoriasis. These are more precise than older drugs, but they’re also more expensive and can raise infection risk. Other common types include calcineurin inhibitors like cyclosporine and tacrolimus, which are critical for transplant patients, and antimetabolites like azathioprine that interfere with immune cell growth.
These drugs don’t work the same for everyone. A dose that keeps one person’s transplant safe might leave another vulnerable to infection. That’s why regular blood tests and close doctor visits are part of the routine. Some people need to take these drugs for life. Others, like those with temporary flare-ups of lupus or multiple sclerosis, might only need them for months. What’s clear is that stopping them without medical advice can lead to organ rejection or a severe disease relapse. And while they’re lifesavers, they’re not without trade-offs—higher risk of infections, certain cancers, and long-term organ damage are real concerns.
You’ll find posts here that dig into how these drugs interact with other medications—like how quercetin supplements can interfere with liver enzymes that break down immunosuppressants, or how proton pump inhibitors can affect how well antiplatelet drugs work alongside them. There’s also coverage of real-world challenges: how patent delays impact access to affordable versions, why generic lithium requires careful monitoring (a similar principle applies to some immunosuppressants), and how genetic differences affect drug metabolism. Whether you’re a patient, caregiver, or just trying to understand why someone needs to take so many pills every day, this collection gives you the facts without the fluff.