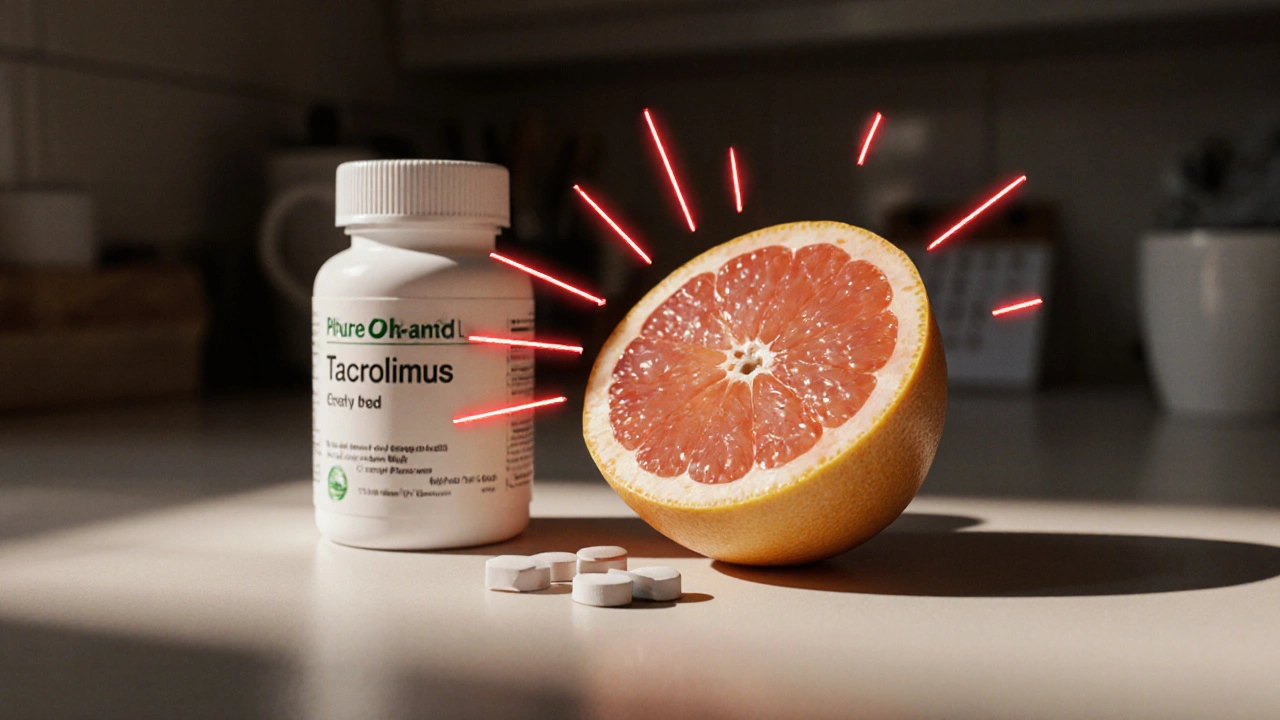
One half of a grapefruit might seem harmless-maybe even healthy. It’s full of vitamin C, fiber, and antioxidants. But if you’re taking an immunosuppressant after a transplant, that small fruit could land you in the hospital. This isn’t a myth. It’s a well-documented, life-threatening interaction that’s been known since 1989. And it doesn’t take much to trigger it.
Why Grapefruit Is Dangerous With Immunosuppressants
Grapefruit doesn’t just interact with some medications-it can dramatically change how your body handles them. The problem lies in a group of chemicals called furanocoumarins, found in grapefruit, pomelo, and Seville oranges. These compounds don’t just slow down drug metabolism-they shut it down completely, at least for a while. Your body uses an enzyme called CYP3A4 to break down many drugs as they pass through your gut. This enzyme acts like a filter, keeping drug levels from getting too high. But grapefruit’s furanocoumarins bind permanently to CYP3A4 in your intestines, disabling it. When that filter is gone, up to 300% more of your medication enters your bloodstream. For immunosuppressants like cyclosporine, tacrolimus, and sirolimus, this is catastrophic. These drugs already have a razor-thin safety margin. The difference between the right dose and a toxic one is small-sometimes just 2 to 4 times higher. A normal level of tacrolimus might be 8 ng/mL. After grapefruit? It can jump to 20 ng/mL or more. That’s not just elevated-it’s dangerous.Which Immunosuppressants Are Affected?
Not all immunosuppressants react the same way. But the ones most commonly used after organ transplants are the most vulnerable:- Cyclosporine (Sandimmune, Neoral): Grapefruit can raise blood levels by 50-100%. Toxic levels start above 500 ng/mL. Normal range: 100-400 ng/mL.
- Tacrolimus (Prograf, Envarsus XR, Astagraf XL): Levels can spike 30-50%, sometimes doubling. Toxic threshold: over 20 ng/mL. Normal: 5-15 ng/mL.
- Sirolimus (Rapamune): One study showed levels jumping 200-300% after grapefruit juice. Normal range: 4-12 ng/mL.
- Everolimus (Zortress): Added to the high-risk list in 2023 by the American Society of Health-System Pharmacists.
How Long Does the Effect Last?
This isn’t a matter of avoiding grapefruit on the same day you take your pill. The damage lasts for days. A 2005 study in Clinical Pharmacology & Therapeutics showed that even after 72 hours, CYP3A4 activity was still reduced by 24%. That means if you drink grapefruit juice on Monday, your body is still vulnerable on Thursday. Taking your immunosuppressant on Thursday? You’re still at risk. That’s why transplant centers require patients to avoid grapefruit for at least three full days before starting any new medication-or even before changing doses. It’s not enough to skip it the morning of your dose. You need to cut it out completely.What Counts as “Grapefruit”?
It’s not just the fruit. It’s not even just the juice.- Grapefruit juice (even small amounts): As little as 200 mL (under one cup) can trigger a reaction.
- Whole grapefruit: The flesh and peel contain the same furanocoumarins.
- Grapefruit extracts or supplements: Often sold as “weight loss aids” or “detox” products-these are especially dangerous because they’re concentrated.
- Pomelo: A larger citrus relative of grapefruit. Same chemicals. Same risk.
- Seville oranges: Used in marmalade. Often mistaken for sweet oranges. These contain the same enzyme-blocking compounds.

What Happens When Levels Get Too High?
Too much immunosuppressant doesn’t make you stronger-it makes you weaker in dangerous ways.- Severe kidney damage: Cyclosporine and tacrolimus are toxic to kidneys at high levels. Many patients end up with acute kidney injury requiring dialysis.
- Increased infection risk: Over-suppressing your immune system leaves you vulnerable to pneumonia, sepsis, and even rare fungal infections.
- Neurotoxicity: Tremors, headaches, seizures, and confusion are signs your brain is being affected.
- High blood pressure: A common side effect that spikes dangerously with elevated drug levels.
- Hyperkalemia: Potassium levels rise, which can trigger irregular heart rhythms.
How Common Is This Problem?
About 300,000 people in the U.S. are on immunosuppressants after transplants. Nearly all of them take drugs affected by grapefruit. And yet, studies show 25% of transplant patients still consume it regularly. Why? Lack of awareness. A 2023 survey by the British Liver Trust found that 68% of transplant patients didn’t fully understand the risk. Many think “a little won’t hurt.” Others assume their doctor told them. Some say they forgot. One patient told researchers, “I thought it was just for blood pressure meds.” This isn’t just about forgetting. It’s about misinformation. Grapefruit is marketed as a “superfood.” People eat it for weight loss, detox, or heart health. But for transplant patients, that health benefit comes at the cost of their transplant’s survival.What Should You Do?
There’s only one safe answer: avoid grapefruit and its close relatives entirely.- Read your medication guide. The FDA requires all cyclosporine and tacrolimus packaging to include a bolded warning: “CONCOMITANT USE WITH GRAPEFRUIT IS CONTRAINDICATED.”
- Ask your pharmacist. They’re trained to spot these interactions. Don’t assume your doctor told you everything.
- Check all products. Some smoothies, salad dressings, and supplements contain grapefruit extract. Read ingredient lists.
- Set phone reminders. If you used to eat grapefruit daily, make a habit of reminding yourself: “No grapefruit. Ever.”
- Use the Johns Hopkins app. Launched in January 2023, it scans your medication barcode and instantly flags grapefruit risks.