Gentamicin Kidney Damage: What You Need to Know About This Common Antibiotic Risk
When your body fights a serious infection, gentamicin, a powerful antibiotic in the aminoglycoside class used to treat life-threatening bacterial infections like sepsis and pneumonia. Also known as an aminoglycoside antibiotic, it works fast—but it doesn’t care if it’s killing bacteria or damaging your kidneys. That’s why gentamicin kidney damage is one of the most well-documented side effects in clinical use. It’s not rare. It’s predictable. And if you’re on it, you need to know the signs before it’s too late.
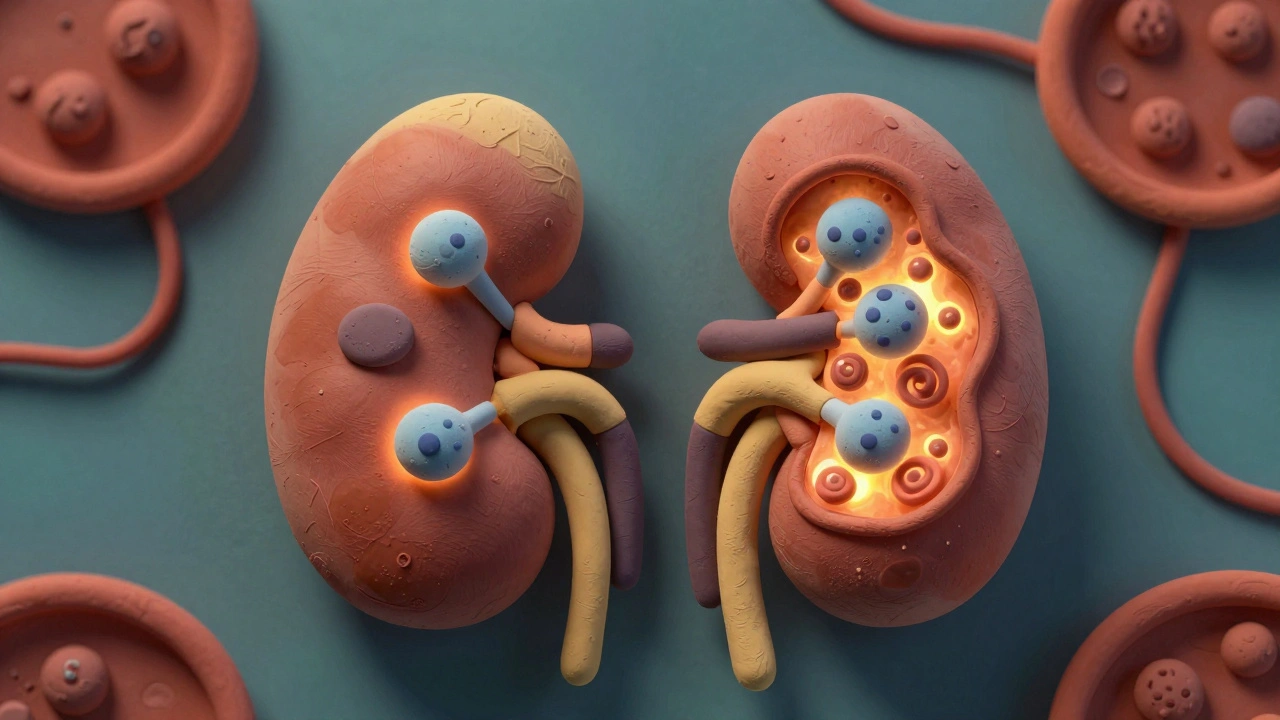
This isn’t just about one drug. nephrotoxicity, the technical term for kidney damage caused by medications is a real concern with aminoglycoside antibiotics, a group that includes gentamicin, tobramycin, and amikacin. These drugs build up in the kidney’s filtering cells, especially if you’re dehydrated, older, or already have reduced kidney function. The damage starts quietly—maybe just a slight drop in urine output or a small rise in creatinine levels—but it can spiral into acute kidney injury if not caught early. Doctors check blood levels of gentamicin and track kidney function daily when it’s given, because the window between effective dose and toxic dose is narrow.
It’s not just the drug itself. Things like taking other kidney-stressing meds—NSAIDs, certain blood pressure pills, or even contrast dye for scans—can make gentamicin damage worse. People in intensive care, those with cystic fibrosis, or anyone on long courses of treatment are at higher risk. Even short courses can cause harm if you’re not monitored. The good news? Most kidney damage from gentamicin is reversible if caught fast. Stopping the drug, staying hydrated, and switching to a safer antibiotic often lets the kidneys heal.
What you’ll find below are real, practical posts that dig into how drugs like gentamicin affect the body, what doctors look for, and how other medications interact with kidney health. You’ll see how ACE inhibitors can be risky in people with kidney issues, why grapefruit changes how drugs like immunosuppressants behave, and how even something as simple as food timing can change how your body handles medicine. These aren’t theory pieces—they’re based on clinical patterns, patient outcomes, and real-world pharmacy practice. If you’re on gentamicin, or know someone who is, this collection gives you the facts you need to ask the right questions and stay safe.