When a generic drug hits the market, it’s not set in stone. Even small tweaks to how it’s made can trigger a full regulatory review by the FDA. For manufacturers, this isn’t just paperwork-it’s time, money, and sometimes, market access on the line. So what exactly makes the FDA step in and demand a re-evaluation? It all comes down to manufacturing changes that could affect the drug’s safety, strength, purity, or quality.
Why the FDA Cares About Manufacturing Changes
Generic drugs don’t need to repeat the same clinical trials as brand-name drugs. That’s the whole point of the Abbreviated New Drug Application (ANDA) process. But there’s one rule: the generic must be bioequivalent to the Reference Listed Drug (RLD). If you change how it’s made-whether it’s the equipment, the process, or the ingredients-the FDA has to check if that still holds true. It’s not about making the drug better. It’s about making sure it’s the same. Even a change in the tablet press, a new supplier for an inactive ingredient, or moving production to a different factory can trigger a re-evaluation. The FDA doesn’t assume the change is harmless. They require proof.The Three Types of Manufacturing Change Submissions
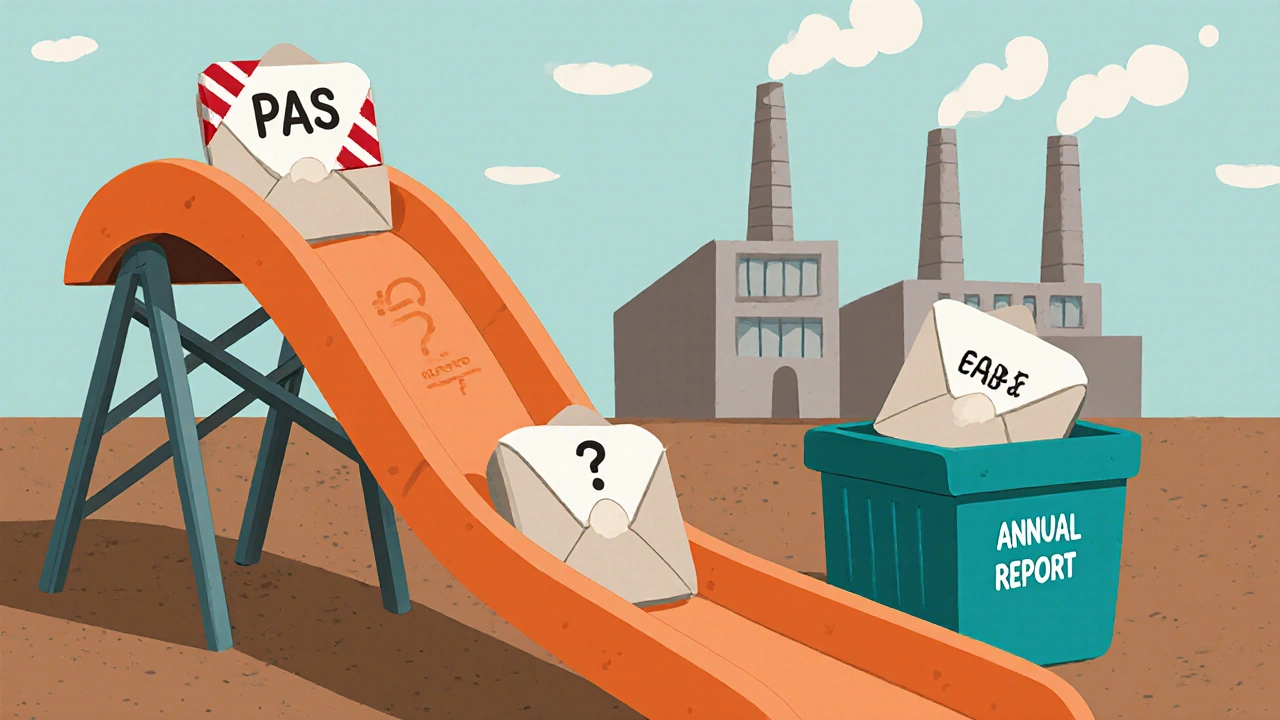
Not every change needs the same level of review. The FDA classifies post-approval changes into three categories, based on risk:- Prior Approval Supplements (PAS): These are the big ones. You can’t make the change until the FDA says yes. This applies to major changes like switching to a new synthetic route for the active ingredient, changing the manufacturing facility, or altering the drug’s formulation in a way that could affect how it’s absorbed.
- Changes Being Effected (CBE): You can make these changes immediately, but you must notify the FDA within 30 days. This is for moderate-risk changes, like updating an analytical method or adjusting in-process controls.
- Annual Reports (AR): The lowest risk. These are minor changes, like updating labeling or changing packaging materials. You just report them in your yearly summary.
Between 2018 and 2022, PAS submissions rose by 27.3%. Why? More companies are upgrading equipment, moving production to the U.S., or adopting continuous manufacturing. But many changes aren’t planned-they’re forced by out-of-spec results, supply chain breaks, or failed batches.
What Changes Most Often Trigger a Full Review?
Some changes are red flags every time. Here are the top triggers based on FDA data from 2018-2023:- Facility transfers: Moving production from one plant to another-even if it’s the same company-requires a PAS. The FDA needs to inspect the new site and confirm the product is identical.
- Changes to the active ingredient source: Switching from one API manufacturer to another? That’s a PAS. Even if the chemical is the same, impurities or crystal structure can differ.
- Formulation changes: Adding or removing an excipient, changing the binder, or altering the coating can affect how the drug dissolves. That’s a bioequivalence issue.
- Scale-up or scale-down: Making 10,000 tablets a day vs. 100,000? The mixing, drying, and compression behavior can change. You need validation data to prove it doesn’t affect performance.
- Process changes: Switching from batch to continuous manufacturing? That’s a game-changer. The FDA requires full comparative studies, even if the end product looks identical.
For complex generics-like injectables, inhalers, or peptides-the rules are even tighter. A new impurity above 0.5%? You need to prove it doesn’t harm patients. The FDA’s 2021 guidance on peptide impurities shows how specific they’ve become.
How Long Does a Re-Evaluation Take?
The timeline varies wildly depending on the type of submission:- PAS: Average 10 months, but complex cases can take 14-18 months. One company reported a 30% batch size increase took 14 months to approve.
- CBE-30: 3 months for FDA to respond.
- CBE-0: 9 months, but you can implement the change immediately.
And here’s the catch: 68.4% of PAS submissions get a complete response letter-meaning the FDA asks for more data. The most common reasons? Analytical method changes (28.7%), facility transfers (24.5%), and formulation updates (19.3%).
Small manufacturers feel this the hardest. A 2023 survey found companies with fewer than 5 ANDAs took 43% longer to get approvals than big players. Why? They lack dedicated regulatory teams and struggle to predict what the FDA will ask for.
How Companies Are Fighting Back
Smart manufacturers aren’t waiting for the FDA to catch them off guard. They’re building flexibility into their products from day one.- Quality by Design (QbD): This approach maps out how every variable-temperature, pressure, mixing time-affects the final product. If you understand the “design space,” you can make changes within it without triggering a PAS.
- Process Analytical Technology (PAT): Real-time monitoring during production helps catch issues early. Companies using PAT saw 32.6% fewer PAS submissions over five years.
- Pre-submission meetings: Talking to the FDA before you file? That’s now standard practice. Teva’s amlodipine continuous manufacturing approval took just 8 months because they had 5 pre-submission meetings.
But it’s expensive. The average PAS costs $287,500 to prepare and submit. For a low-margin generic drug, that’s a hard sell. Many companies avoid upgrades altogether, even if they’d improve quality or reduce waste.

The New Rules: Faster Reviews for U.S.-Made Drugs
The FDA is trying to fix this. In September 2023, they launched the ANDA Prioritization Pilot Program. If your generic drug is made in the U.S., uses U.S.-sourced active ingredients, and has U.S.-based bioequivalence data, your review can be cut from 30 months to just 8.This isn’t charity. It’s strategy. Commissioner Robert Califf says the goal is to bring $4.2 billion in new U.S. manufacturing investment by 2027. And it’s working. By 2026, nearly 38% of new generic approvals are expected to qualify.
Another new tool? The PreCheck program. It’s a two-phase review for high-priority facilities. Instead of waiting 18 months for a facility transfer approval, you could get it in 9.
What’s Next?
The next big shift is coming with GDUFA IV, the next round of user fee negotiations in 2025. The industry wants standardized rules for classifying changes. Right now, one FDA division might call a change a PAS, while another says it’s a CBE. That inconsistency creates confusion and delays.McKinsey & Company estimates that by 2030, manufacturers who adopt advanced technologies and smarter change controls could save $8.7 billion a year in lost revenue from delayed approvals.
Bottom line: Manufacturing changes aren’t just technical decisions-they’re regulatory, financial, and strategic ones. The companies that win aren’t the ones with the cheapest production. They’re the ones who understand the rules, plan ahead, and build flexibility into their processes from the start.
What manufacturing changes require FDA approval before implementation?
Changes that significantly affect the drug’s safety, identity, strength, quality, or purity require a Prior Approval Supplement (PAS). This includes switching manufacturing facilities, changing the active ingredient supplier, altering the drug formulation, or moving from batch to continuous manufacturing. You cannot implement these changes until the FDA approves your submission.
Can I change the tablet press without notifying the FDA?
No. Even if the tablet looks the same, changing the tablet press can affect hardness, dissolution, and uniformity. If the change impacts critical quality attributes, it likely requires a PAS or at minimum a CBE-30. You must validate the new equipment and compare pre- and post-change batches. Never assume a mechanical change is too small to matter.
How do I know if my change is a PAS, CBE, or Annual Report?
Start with the FDA’s 2011 guidance on post-approval changes. Use a risk-based assessment: Will this change affect bioequivalence? Could it introduce new impurities? Will it alter how the drug is absorbed? If the answer is yes, it’s likely a PAS. If it’s a minor analytical update or labeling change, it may be a CBE or Annual Report. When in doubt, request a pre-submission meeting with the FDA.
Why do some companies avoid making manufacturing improvements?
Because the cost and delay of a PAS can outweigh the benefits. For a low-margin generic drug, spending $287,500 and waiting 14 months for approval isn’t worth it-even if the new process is more efficient or sustainable. Many manufacturers choose to stick with outdated equipment rather than risk regulatory delays or supply disruptions.
Does the FDA inspect facilities before approving a manufacturing change?
Yes, especially for PAS submissions involving new facilities or major process changes. The FDA often requires an inspection before approval. Even if your facility was inspected before, a new change can trigger a fresh inspection. Companies with strong quality systems and clean inspection histories see faster approvals.
What’s the fastest way to get a manufacturing change approved?
Apply for the FDA’s ANDA Prioritization Pilot Program. If your drug is made in the U.S., uses U.S.-sourced active ingredients, and has U.S.-based bioequivalence data, you can get approval in as little as 8 months. Pre-submission meetings, robust data packages, and using Quality by Design principles also speed things up.
What Should You Do Next?
If you’re managing a generic drug product:- Map out every manufacturing change you’ve made in the last two years. Were they properly classified?
- Review your change control system. Does it include a risk assessment step before any change is made?
- Check if your facility qualifies for the ANDA Prioritization Pilot Program. If yes, start gathering the required documentation.
- Consider investing in Quality by Design or PAT tools. They reduce long-term regulatory risk.
- Don’t wait for a problem to happen. Proactively reach out to the FDA for pre-submission meetings if you’re planning a major change.
The system isn’t perfect. But it’s not impossible. The companies that thrive are the ones who treat regulatory compliance not as a cost center, but as a strategic advantage.

