Warfarin Genetics: How Your DNA Affects Blood Thinners
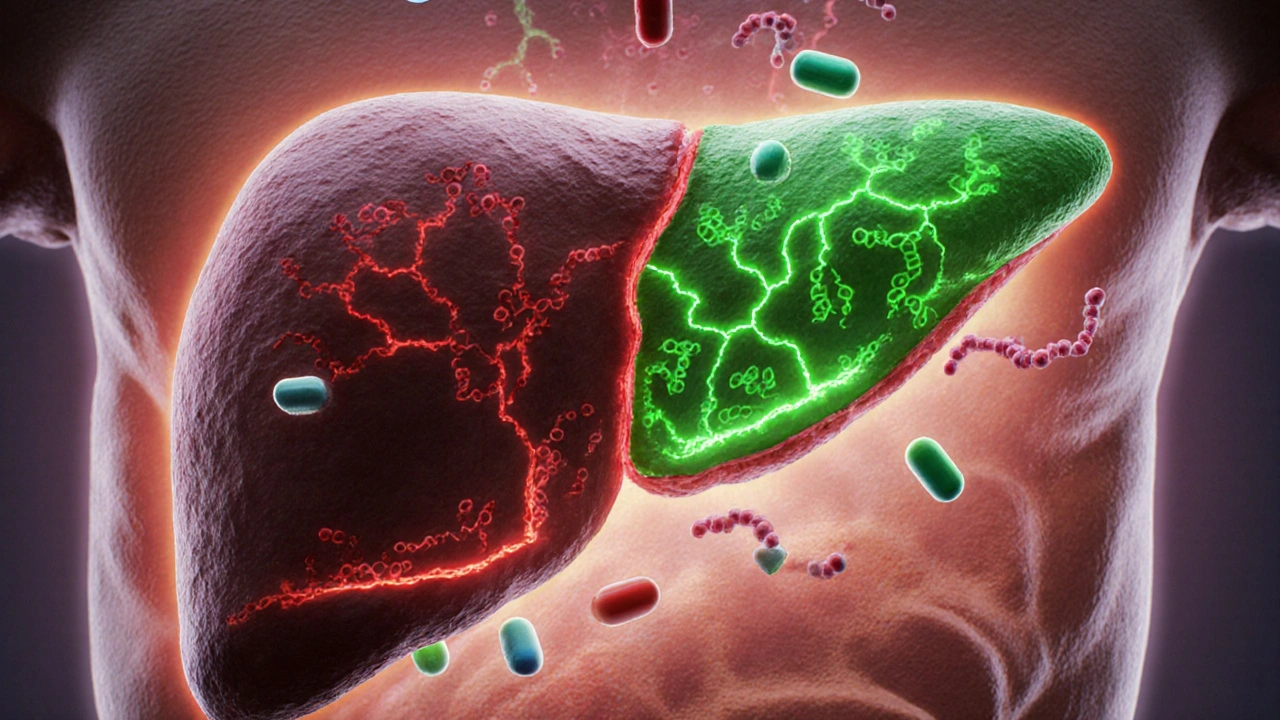
When you take warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. Also known as Coumadin, it's one of the most commonly prescribed anticoagulants—but it doesn't work the same for everyone. Two genes, CYP2C9, a liver enzyme that breaks down warfarin, and VKORC1, a gene that controls how sensitive your blood is to warfarin, determine how fast your body clears the drug and how strongly it reacts. If you have a slow-metabolizing version of CYP2C9, even a standard dose can build up to dangerous levels. If your VKORC1 gene makes you super-sensitive, you might bleed from a dose that works fine for someone else.
This isn't theoretical. Studies show that up to 40% of warfarin dosing variability comes from these two genes alone. Doctors used to guess the right dose based on age, weight, and diet—often leading to hospital visits from bleeding or clots. Now, genetic testing can tell you upfront whether you're a low, medium, or high responder. It’s not magic, but it’s science that saves lives. Someone with two slow CYP2C9 variants might need just 1 mg a day, while someone with fast metabolism might need 7 mg or more to get the same effect. That’s a seven-fold difference. And getting it wrong? It can mean a stroke, a brain bleed, or worse.
The good news? You don’t need to guess anymore. If you're on warfarin—or thinking about starting it—knowing your genetic profile can cut down the trial-and-error phase from weeks to days. It’s especially helpful for older adults, people with liver issues, or those who’ve had bad reactions before. While not every clinic offers testing yet, more insurers are covering it because it reduces overall costs and complications. And if you’ve ever been told your INR was "all over the place" despite sticking to your diet and schedule, your genes might be the real reason.
Below, you’ll find real-world posts that connect warfarin genetics to broader topics like pharmacogenomic testing, drug interactions, and how genes affect other medications like SSRIs and antibiotics. These aren’t abstract studies—they’re practical guides from people who’ve lived through it, doctors who’ve seen the results, and patients who finally got it right after years of trial and error.