Midodrine and Physical Activity: What You Need to Know
When you take midodrine, a medication used to treat low blood pressure, especially when standing up. It works by tightening blood vessels to raise blood pressure and prevent dizziness or fainting. Many people on midodrine wonder if they can still be active — walking, lifting weights, or even just doing housework — without risking side effects. The answer isn’t simple, but it’s practical: yes, you can stay active, but you need to understand how midodrine interacts with your body during movement.
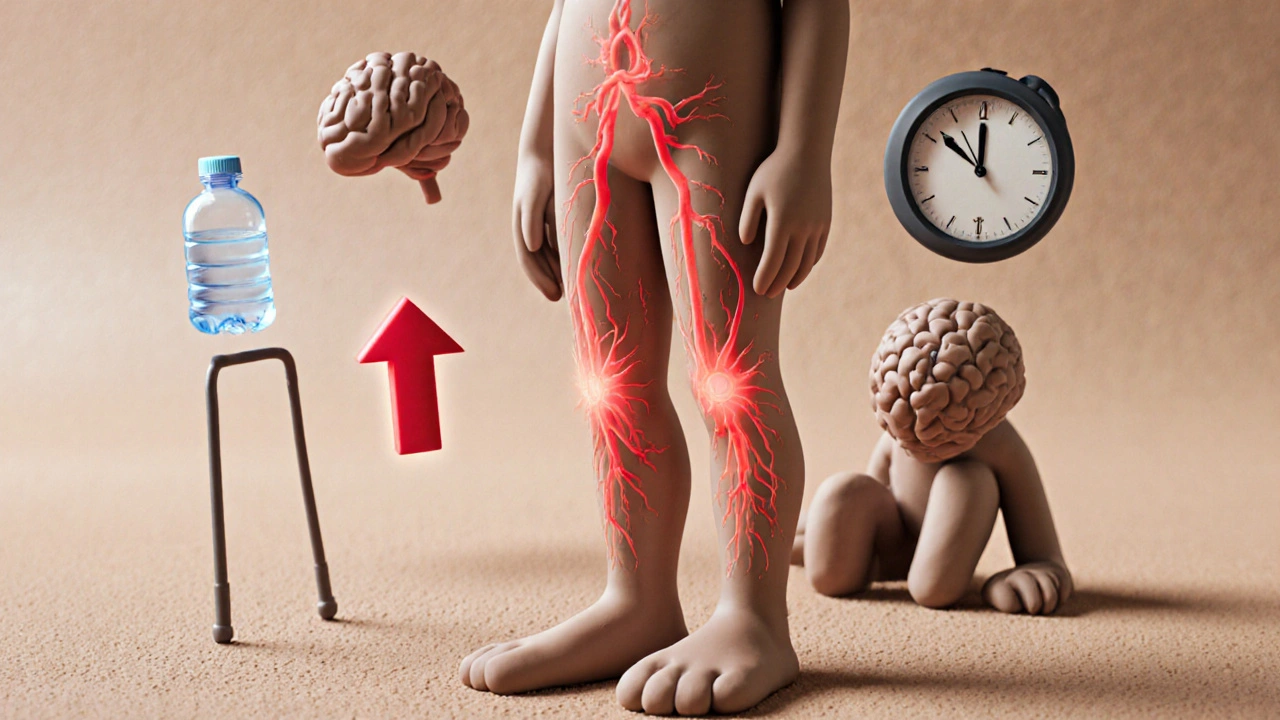
Physical activity, any movement that increases heart rate and muscle use naturally changes your blood pressure. When you stand up or start moving, gravity pulls blood down, and your body usually responds by constricting vessels to keep blood flowing to the brain. But if you have orthostatic hypotension, a condition where blood pressure drops too much when standing, that natural response fails. That’s where midodrine helps — it gives your blood vessels a boost. But if you’re active, especially during or right after taking your dose, your blood pressure can spike too high. This isn’t just about feeling lightheaded — it’s about avoiding dangerous highs that strain your heart or cause headaches, blurred vision, or even stroke risk.
People who take midodrine often report feeling fine sitting still but getting a pounding headache or racing heart after a short walk. That’s not normal fatigue — it’s a sign your body’s pressure regulation is being pushed too far. Timing matters. Most doctors recommend taking midodrine 30 minutes before getting up, and avoiding intense activity within 4 to 6 hours after your last dose. Light activity like slow walking or stretching is usually fine, but lifting heavy weights, sprinting, or hot yoga? Those can be risky. Also, stay hydrated. Dehydration makes low blood pressure worse, and midodrine doesn’t fix that — it just tightens vessels, which can backfire if you’re low on fluids.
It’s not just about the drug and the workout — it’s about your whole routine. If you’re on midodrine because of autonomic nervous system issues — maybe from diabetes, Parkinson’s, or aging — your body’s ability to adjust to movement is already limited. That means you need to be extra careful. Monitor your blood pressure before and after activity. Keep a log. Notice patterns. Does your pressure jump after climbing stairs? Does your head throb after gardening? These aren’t just inconveniences — they’re signals your body is under stress.
There’s no one-size-fits-all rule. Some people handle moderate activity well. Others need to keep things very gentle. The goal isn’t to stop moving — it’s to move safely. Talk to your doctor about your activity level. Ask for a simple plan: what’s safe, what to avoid, and when to check your pressure. You don’t have to sit on the couch. But you do need to know how your body reacts — because midodrine gives you control, but only if you use it wisely.
Below, you’ll find real-world insights from people managing this balance — from how midodrine affects heart rate during exercise, to what happens when you skip a dose before walking the dog, to the subtle signs that tell you it’s time to slow down. These aren’t theory pages. They’re lived experiences, backed by clinical understanding, and meant to help you move with confidence — not fear.